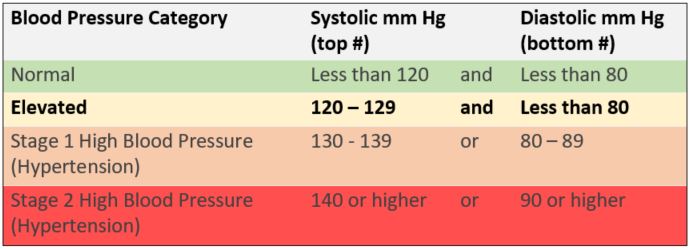
According to 2017 hypertension guidelines from the American College of Cardiology and American Heart Association (ACC/AHA), doctors should treat people with elevated blood pressure (BP).1 This is now a new category that is distinct from the diagnosis of high blood pressure. The experts determined that lower treatment thresholds and targets will benefit patients who have a higher than normal risk of blood pressure-related complications, such as heart attack, heart failure, and stroke.1-4
The risk for heart attack, stroke and other high blood pressure complications begins to increase around 115/75 mm Hg.1,2,4-6 The risk doubles for each 20 mm Hg increase in the systolic pressure and each 10 mm Hg increase in the diastolic pressure. Although people with elevated blood pressure (120 to 129 mm Hg systolic and less than 80 mm Hg diastolic) may only be starting to have slightly increased risk, adopting healthy lifestyle habits may prevent progression to high blood pressure and the associated increased risk of hypertension-related diseases.1
Doctors should promote nonpharmacological therapy to people with elevated BP and reassess them in three to six months to see if lower BP goal is met.1 Nonpharmacological therapy includes healthy diet, weight loss, sodium reduction, exercise, enhanced intake of dietary potassium, and moderating alcohol consumption. Doctors should consider out-of-office BP measurement using 24-hour ambulatory blood pressure monitoring (ABPM) or self-measured blood pressure (SMBP) at home to confirm elevated BP and check for masked hypertension.
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.
- Reboussin DM, Allen NB, Griswold ME, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017.
- Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA 2017; 318 (21): 2132-2134.
- Wright JT, Jr., Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373 (22): 2103-2116.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360 (9349): 1903-1913.
- Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383 (9932): 1899-1911.

.png)