Manufacturers’ of statins state that patients who drink substantial amounts of alcohol or who have chronic liver disease should use caution if they take statins.1-7 They also state that patients with chronic alcoholic liver disease have modest1 to markedly2 increased plasma concentrations of the statin. Patients with active liver disease should not take statins.1-7
Rarely, cases of liver failure attributed to statins have been reported, so regular liver function tests are recommended by the manufacturers for all people taking a statin.1-7 However, in randomized controlled trials there was no significant difference in the incidence of increased liver enzymes when statins and placebos were compared.8-10
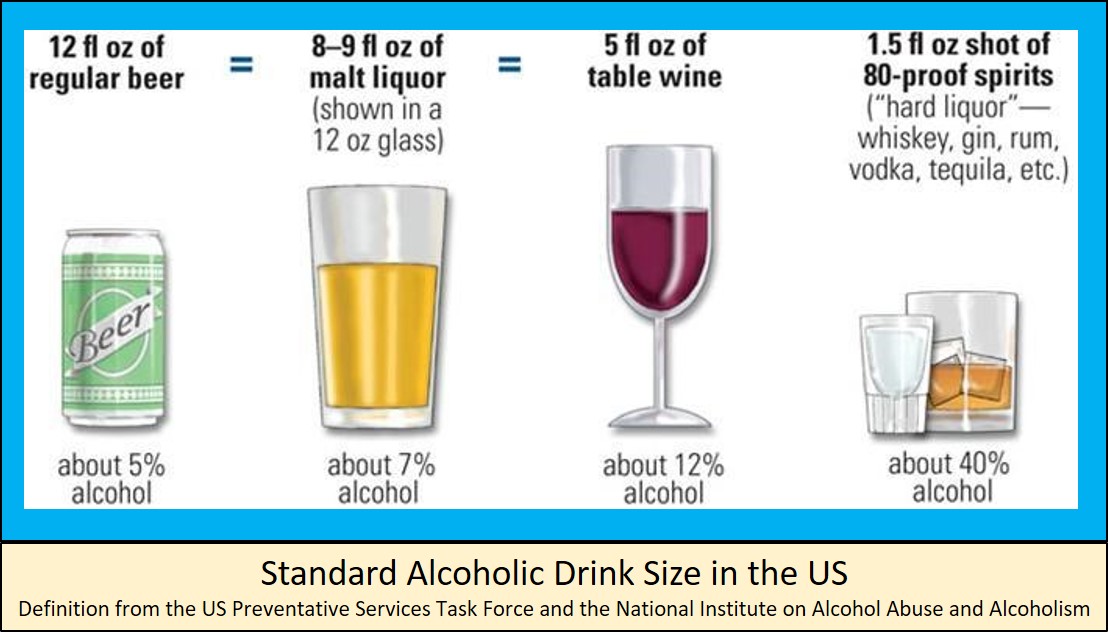
The risk of liver injury may be higher when someone with heavy alcohol consumption also takes statins. This is because liver damage is also common with heavy alcohol consumption. Hepatosteatosis (fatty liver disease) develops in about 20% of all alcoholics and heavy drinkers.11 There are usually no symptoms and the problem can be reversed if alcohol use is stopped or lowered significantly. Alcoholic hepatitis occurs when changes to the liver such as inflammation, fibrosis, or degeneration that can be seen on biopsy occur. When people develop this, they often have symptoms. It can result in death in severe cases and progress to cirrhosis if heavy drinking continues. Cirrhosis is the result of most chronic liver disease. It occurs when scar tissue replaces healthy liver tissue. About 10% to 15% of heavy drinkers eventually develop cirrhosis. The Dietary Guidelines for Americans 2015-2020 states that if alcohol is consumed, it should be in moderation—up to one drink per day for women and up to two drinks per day for men—and only by adults of legal drinking age. For those who choose to drink, moderate alcohol consumption is recommended.12
The manufacturers’ patient information for statins instructs patients to tell their doctor if they drink two or more glasses of alcohol per day.1,2,5 Patients should limit drinking excessive quantities of alcohol while taking statins to avoid hepatotoxicity. Patients who are heavy alcohol drinkers should be closely monitored for hepatotoxicity while on a statin.5
References
- Rosuvastatin [package insert]. Weston, FL: Apotex Corp.; 2019.
- Lipitor - atorvastatin calcium [package insert]. New York, NY: Parke-Davis Division of Pfizer Inc.; 2019.
- Simvastatin [package insert]. Durham, NC: Accord Healthcare, Inc.; 2018.
- Lovastatin [package insert]. Parsippany, NJ: Actavis Pharma, Inc.; 2017.
- Fluvastatin [package insert]. North Wales, PA: Teva Pharmaceuticals USA, Inc.; 2017.
- Pravastatin [package insert]. Mahwah, NJ: Glenmark Pharmaceuticals Inc., USA; 2016.
- Livalo - pitavastatin calcium [package insert]. Montgomery, AL: Kowa Pharmaceuticals America, Inc.; 2016.
- Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998; 279 (20): 1615-1622.
- Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344 (8934): 1383-1389.
- MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360 (9326): 7-22.
- Mann RE, Smart RG, Govoni R. The epidemiology of alcoholic liver disease. Alcohol Res Health 2003; 27 (3): 209-219.
- 2015 – 2020 dietary guidelines for Americans. 8 ed: U.S. Department of Health and Human Services and U.S. Department of Agriculture; 2015.

.png)