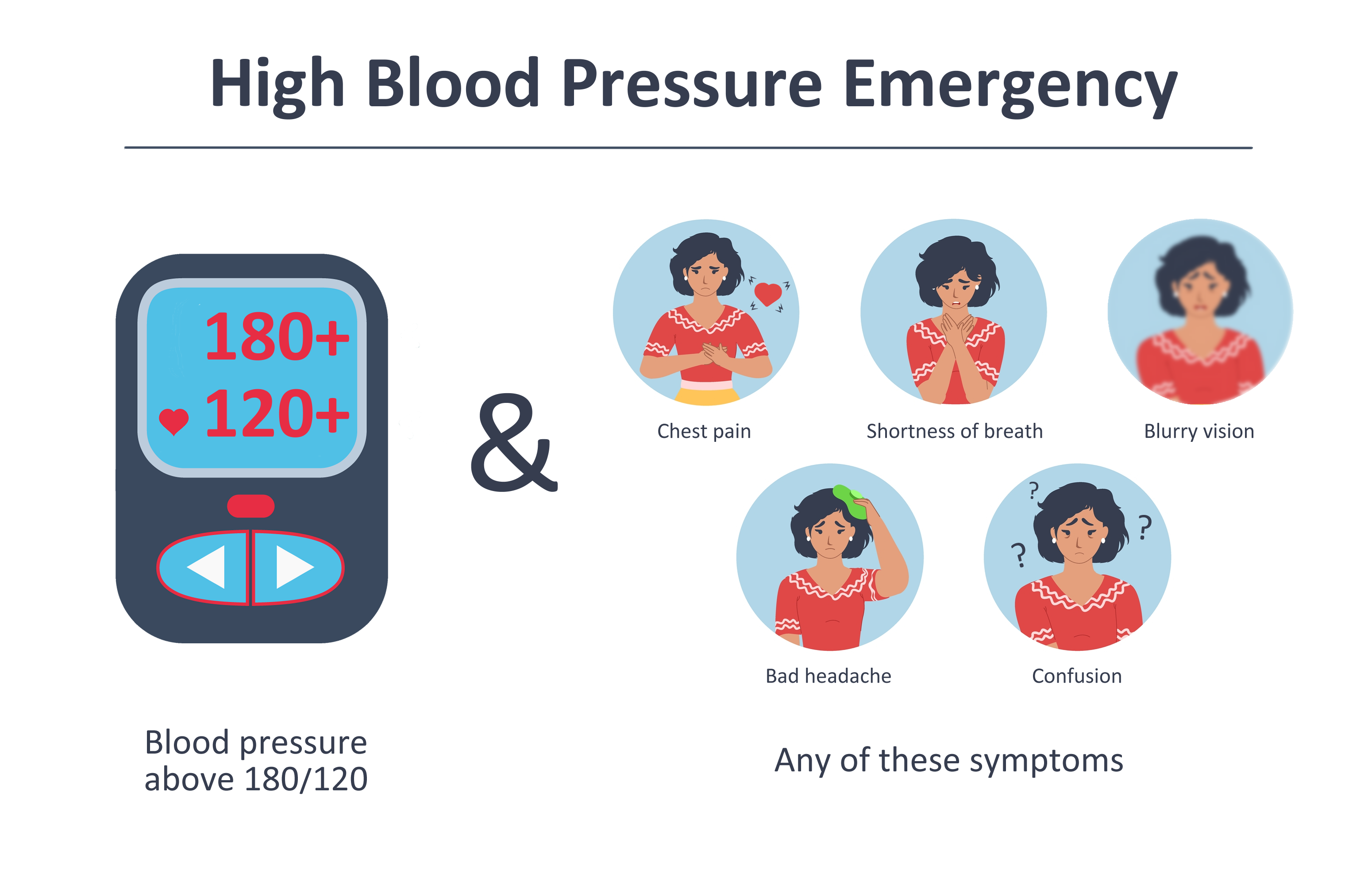
A hypertensive crisis is defined as a severely elevated blood pressure (BP) of 180/120 mmHg or higher.1 A hypertensive emergency is defined as hypertensive crisis with evidence of acute organ damage.2,3 Immediate emergency care becomes necessary in the case of a hypertensive emergency. Patients with a blood pressure greater than 180/120 mmHg without evidence of new organ damage are classified as asymptomatic markedly elevated BP, sometimes referred to as hypertensive urgency.2 Recommendations are inconsistent regarding the requirement of emergency treatment for hypertensive urgency. One view is that patients may be unable to differentiate between a hypertensive emergency and hypertensive urgency, making it imperative to recommend that patients seek treatment if they suspect a hypertensive crisis regardless of symptom status. Others advise that patients can discern the presence of symptoms and should only be counseled to seek treatment when their BP is both severely elevated and they are experiencing symptoms.
The literature is clear on emergency care for patients with hypertensive emergency. Research has shown that nearly 10% of patients admitted with a hypertensive emergency have died during hospitalization, which is why it is essential that these patients are treated with the utmost urgency.4 Studies have further shown that patients with untreated hypertensive emergencies had a one-year mortality rate of around 79%, with median survival of just 10.4 months.3,5 Furthermore, patients with hypertensive emergencies are at risk of end-organ complications affecting the heart, brain, kidneys, eyes, lungs, and blood vessels.1 The most common complications seen are ischemic stroke(28.1%), pulmonary edema/acute heart failure(24.1%), hemorrhagic stroke (14.6%), acute coronary syndrome(10.8%), renal failure(8.0%), subarachnoid hemorrhage(6.9%), encephalopathy (6.1%), and the least prevalent was aortic dissection (1.8%).4
Patients suffering from a hypertensive emergency often experience specific symptoms. The most common symptoms reported by patients are neurological symptoms(35%), dyspnea(31%), and chest pain.6 Patients may also present with neurological complications such as seizures, epilepsy, stroke, or delirium.4 In contrast, patients with asymptomatic markedly elevated BP experience more non-specific symptoms(48%) and headache(22%).6
Cardiac, renal, and cerebral comorbidities including but not limited to coronary artery disease(1.654 times), congestive heart failure(2 times), cerebrovascular disease(1.769 times), and chronic kidney disease (2.899 times) increase the risk of hypertensive crisis.1,7 Studies have also shown that unhealthy alcohol use(1.4 times) and, recreational drug use(3.2 times) are also risk factors for having a hypertensive crisis.1,3,7
References
- Gezie H, Azazh A, Melaku B, Gelaye H. Determinants of hypertensive crisis among hypertensive patients at adult emergency departments of public hospitals in Addis Ababa, Ethiopia, 2021: a case–control study. International Journal of Emergency Medicine. 2023/10/09 2023;16(1):68. doi:10.1186/s12245-023-00549-2
- Bress AP, Anderson TS, Flack JM, et al. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. Aug 2024;81(8):e94–e106. doi:10.1161/hyp.0000000000000238
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. Jun 2018;71(6):1269–1324. doi:10.1161/hyp.0000000000000066
- Siddiqi TJ, Usman MS, Rashid AM, et al. Clinical Outcomes in Hypertensive Emergency: A Systematic Review and Meta-Analysis. J Am Heart Assoc. Jul 18 2023;12(14):e029355. doi:10.1161/jaha.122.029355
- Aronow WS. Treatment of hypertensive emergencies. Annals of Translational Medicine. 2017:S5.
- Astarita A, Covella M, Vallelonga F, et al. Hypertensive emergencies and urgencies in emergency departments: a systematic review and meta-analysis. J Hypertens. Jul 2020;38(7):1203–1210. doi:10.1097/hjh.0000000000002372
- Benenson I, Waldron FA, Jadotte YT, Dreker M, Holly C. Risk factors for hypertensive crisis in adult patients: a systematic review. JBI Evidence Synthesis. 2021;19(6):1292–1327. doi:10.11124/jbies-20-00243


.png)
