Rheumatoid arthritis (RA) is a systemic, chronic inflammatory disease that mainly affects the joints.1 Patients with RA should be started on treatment as early as possible to prevent disease progression, joint damage, worsening of symptoms, and extra-articular manifestations such as premature atherosclerosis. The treatment of rheumatoid arthritis follows the treat-to-target (T2T) approach set by the European League Against Rheumatism and also endorsed by the American College of Rheumatology (ACR).2 The main target is to achieve clinical remission, with low-disease activity as an alternative target. Treatment decisions should be made jointly by the patient and the rheumatologist. Multiple factors, including the duration of disease and prior experience with medications, must be considered. In the Boolean-based definition of remission, the patient must satisfy all of the following:3
- tender joint count ≤1
- swollen joint count <1
- C-reactive protein (CRP) ≤1 mg/dl
- patient global assessment ≤1 (on a 0–10 scale)
In the Index-based definition of remission, the patient must have a Simplified Disease Activity Index score of ≤3.3.3 This is the simple addition of the total number of tender and swollen joints, in addition to patient and physician global assessments, and CRP level.
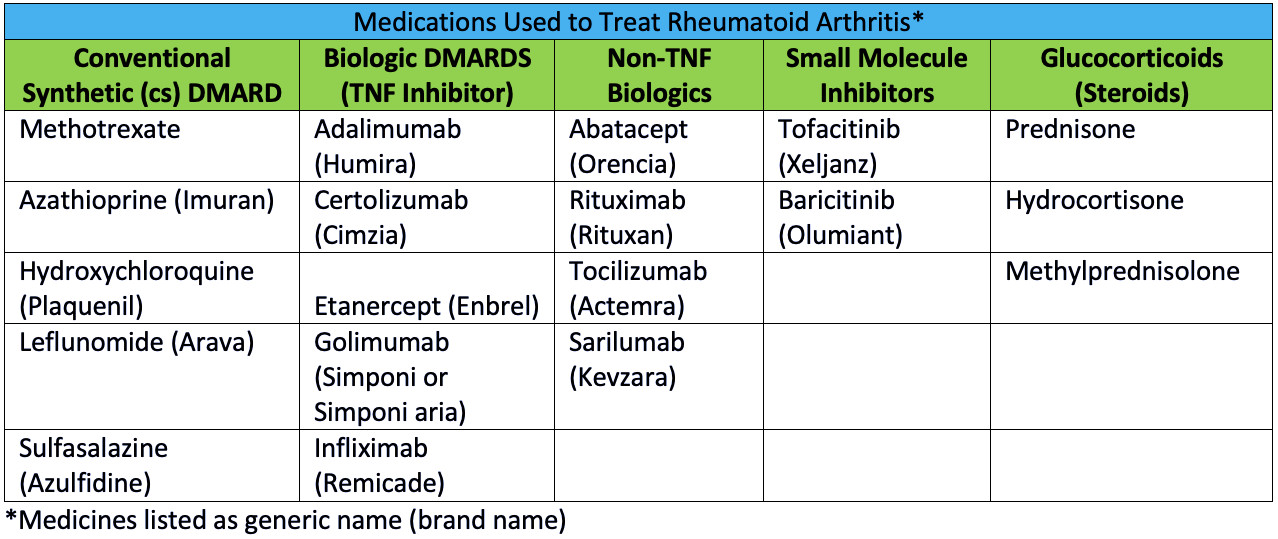
The main type of RA medications are disease-modifying anti-rheumatic drugs (DMARDs).4 The reason that they are called disease-modifying is because they modify and decrease disease progression and the development of joint destruction which can occur untreated RA. DMARDs are divided into 4 groups: conventional synthetic (cs) DMARDs, tumor necrosis factor (TNF) alpha inhibitor biologics, non-TNF inhibitor biologics, and small molecule inhibitors. Medications that are not specific to RA, but are used to help manage inflammation, are glucocorticoids.4 A complete list of these medications is found below.
The ACR recommends methotrexate monotherapy as the first-line therapy for all patients with RA.4 Following monitoring every one to three months by a rheumatologist, treatment may be modified by dose escalation and/or addition of other medications including other csDMARDs, biologic DMARDS, and small molecule inhibitors. Based on disease activity and response, short-term glucocorticoids may also be used at the lowest possible dose.
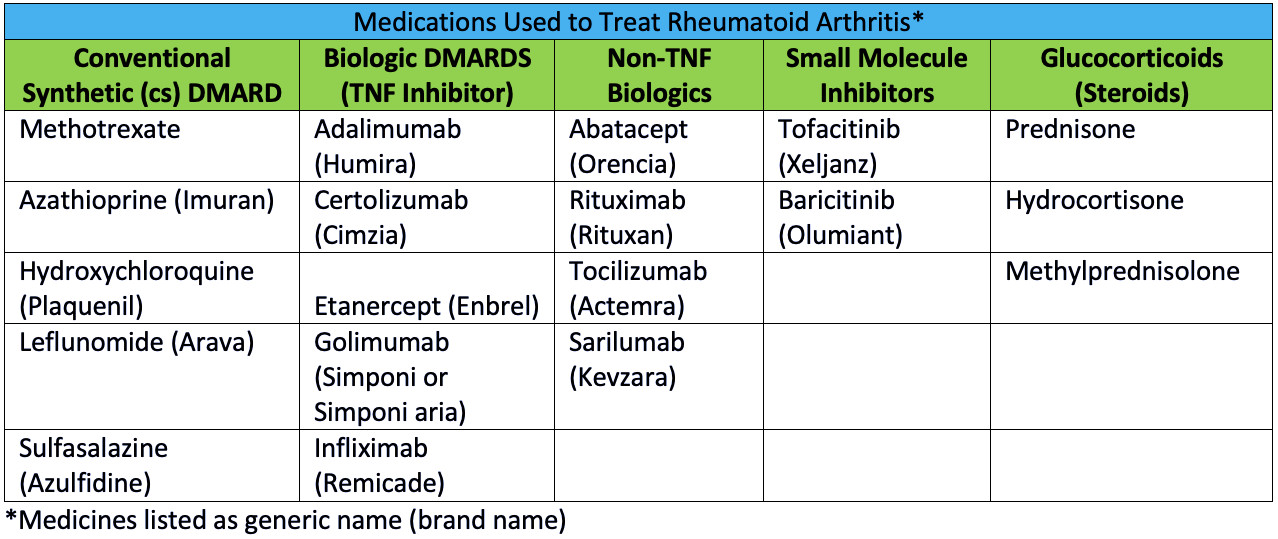 *Medications listed as generic name (brand name)
*Medications listed as generic name (brand name)
References
- Klareskog L, Catrina AI, Paget S. Rheumatoid arthritis. In: Lancet. Vol 373.2009:659-672.
- Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75(1):3-15.
- Felson DT, Smolen JS, Wells G, et al. American college of rheumatology/european league against rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 2011;70(3):404-413.
- Singh JA, Saag KG, Bridges SL, Jr., et al. 2015 american college of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68(1):1-25.
 *Medications listed as generic name (brand name)
*Medications listed as generic name (brand name)