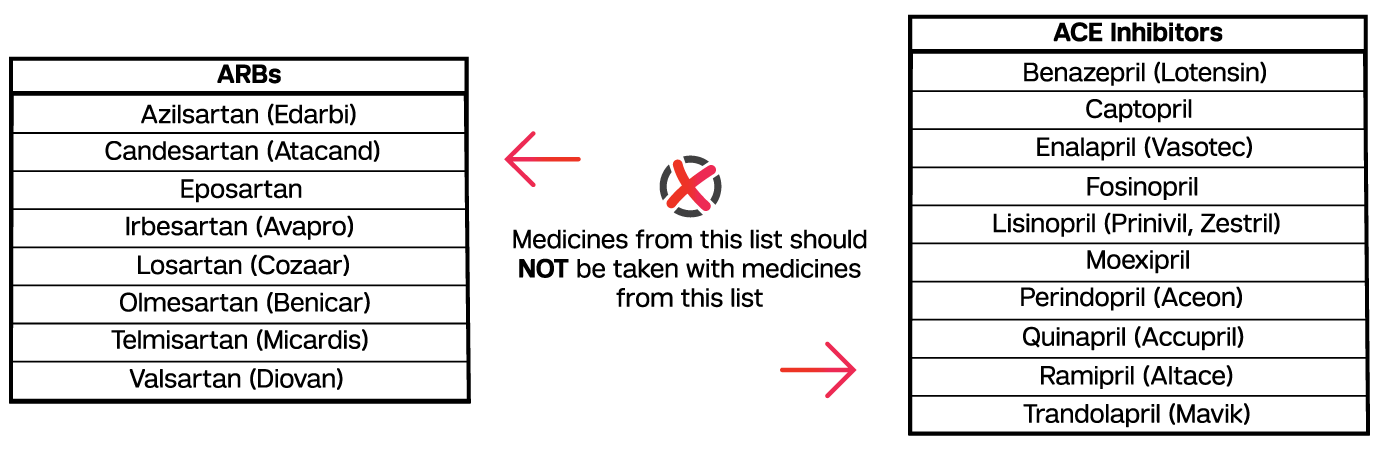
Multiple practice guidelines for the treatment of hypertension recommend against combining an angiotensin-converting enzyme (ACE) inhibitor with an angiotensin-receptor blocker (ARB).1-4
Pfeffer et al. studied the effects of the ARB valsartan, the ACE inhibitor captopril, and the combination of the two on mortality in patients who had an acute myocardial infarction (MI).5 Patients (n=14,703) were men and women 18 years of age and older (mean age=64.8) who had an MI complicated by heart failure (HF), left ventricular systolic dysfunction, or both. Discontinuation of study treatment due to adverse events (hypotension, renal disease, hyperkalemia, cough, rash, taste disturbances, and angioedema) was highest among those in the valsartan-captopril group occurring at a rate of 23.4% compared to 20.5% and 21.6% in the valsartan and captopril monotherapy groups, respectively. At year one, mean systolic blood pressure was 2.2 mm Hg lower in the valsartan-captopril group than in the valsartan and captopril monotherapy groups. Primary outcomes of mortality and cardiovascular morbidity and mortality were similar in all three treatment groups.
In a similar comparative study, Yusuf et al. studied the efficacy of ACE inhibitors, ARBs, and the combination of the two in patients with vascular disease or high-risk diabetes.6 Patients (n=25,620) were 18 years of age and older (mean age=66.45) and were randomized to receive ramipril, telmisartan, or both. With the exception of angioedema, patients receiving combination therapy experienced more adverse events than patients receiving monotherapy. The incidence of death, MI, stroke, and HF in the combination therapy group compared to the ramipril and telmisartan groups was not significantly different (p=0.83). For example, the incidence of death from cardiovascular causes in the ramipril, telmisartan, and combination therapy group were 7, 7, and 7.3%, respectively. These findings suggest there is little to no advantage in using both ACE inhibitors and ARBs for the treatment of cardiovascular disease.
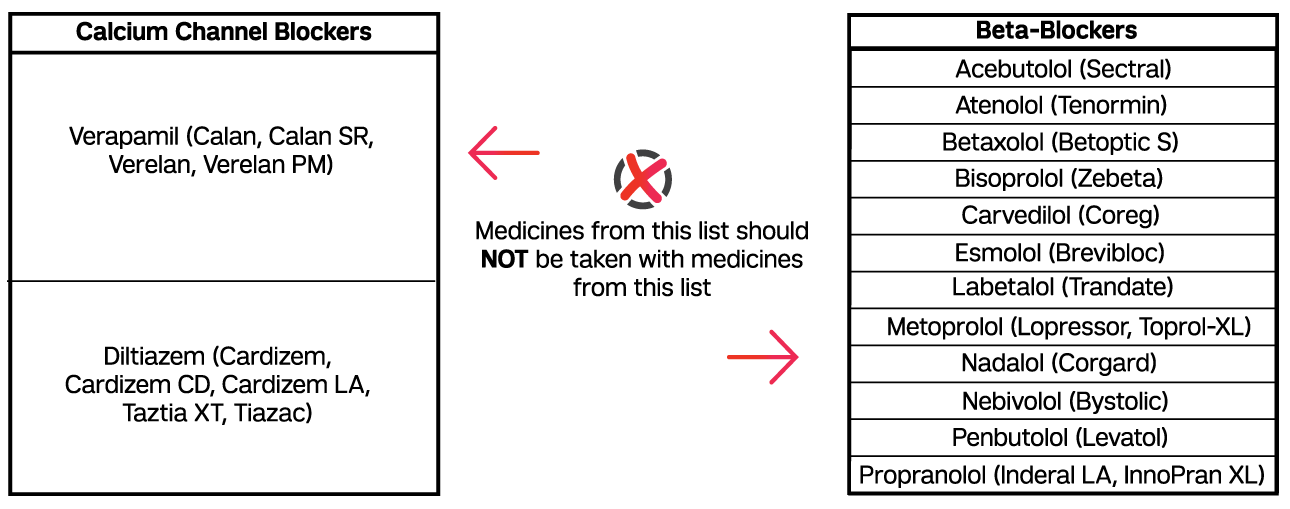
According to the 2017 Hypertension Guidelines, the use of beta blockers with non-dihydropyridine calcium channel blockers (CCBs), verapamil and diltiazem, should be avoided.4 In addition to causing left ventricular depression, beta-blockers can increase the pressor response caused by clonidine withdrawal. The additive effect caused by concomitant use of beta-blockers with non-dihydropyridine CCBs may result in bradycardia.7-9 The European Societies of Hypertension and Cardiology (ESH/ESC) recommend combining beta-blockers with dihydropyridine CCBs.2 Unlike non-dihydropyridine CCBs, which exhibit cardiac selectivity, dihydropyridine CCBs exhibit vascular selectivity and are therefore less negatively inotropic.9
References
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159-2219.
- McCormack T, Krause T, O'Flynn N. Management of hypertension in adults in primary care: NICE guideline. Br J Gen Pract. 2012;62(596):163-164.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017:24430.
- Pfeffer MA, McMurray JJV, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349(20):1893-1906.
- Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. Apr 10 2008;358(15):1547-1559.
- Go AS, Bauman MA, Coleman King SM, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014;63(4):878-885.
- Taddei S. Combination therapy in hypertension: what are the best options according to clinical pharmacology principles and controlled clinical trial evidence? Amer J Cardiovasc Drugs. June 01 2015;15(3):185-194.
- Opie LH. Pharmacological differences between calcium antagonists. Eur Heart J. 1997;18(suppl A):71-79.