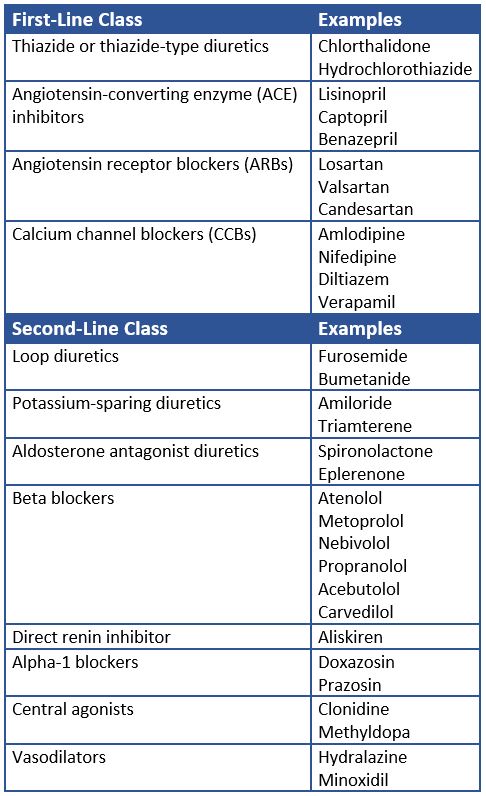
The 2017 hypertension guidelines1 from the American College of Cardiology and American Heart Association (ACC/AHA) recommend many medications and medication classes as oral pharmacological therapy for hypertension:
Primary Agents
- Thiazide or thiazide-type diuretics
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin receptor blockers (ARBs)
- Calcium channel blockers (CCBs)
Secondary Agents
- Loop diuretics
- Potassium-sparing diuretics
- Aldosterone antagonist diuretics
- Beta blockers
- Direct renin inhibitor (Aliskiren)
- Alpha-1 blockers
- Central alpha-agonists
- Direct vasodilators
When to Use Antihypertensives
The 2017 guidelines1 recommend the prescription of a primary antihypertensive medication for all adults with Stage 2 hypertension (140 mm Hg or higher systolic or 90 mm Hg or higher diastolic). People with Stage 1 hypertension (between 130 – 140 mm Hg systolic or 80 – 90 mm Hg diastolic) and either a previous CVD event or an estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk of 10% or higher may also be started on an antihypertensive. All adults with Stage 2 hypertension who have an average blood pressure (BP) more than 20/10 mm Hg above their BP target should be started on two first-line antihypertensive agents from different classes.
The guidelines are slightly different for black adults.1 They state that a thiazide-type diuretic or a calcium channel blocker should be part of initial antihypertensive treatment for black adults with hypertension who do not have heart failure or chronic kidney disease, including those with diabetes mellitus. (Strong Recommendation (Level B – Randomized Trials)]. It also recommends starting adults with hypertension, especially black adults, on two or more antihypertensive medications to help them reach a blood pressure target of less than 130/80 mm Hg. [Strong Recommendation (Level of Evidence C – Limited Data)].
Combination drug therapy can be administered as separate agents or in a fixed-dose combination. People started on one or two antihypertensive drugs should be reassessed within one month. If the blood pressure goal is not met, intensification of therapy with either an increased dose or an additional medication from another antihypertensive class should be considered.
Studies2-4 have shown that starting people on combination drug antihypertensive therapy results in faster blood pressure control compared to monotherapy. More rapid blood pressure control can result in greater risk reduction of cardiovascular (CV) disease.
Intensification of Antihypertensive Drug Treatment
Patients started on one or two antihypertensive medications may still need to increase dosage or add additional medications from other antihypertensive classes to achieve their blood pressure goal.1 Studies have shown that delays in intensification of blood pressure treatment (raised dose or added medications) result in an increased risk of a CV event or death.5
A 2015 retrospective cohort study5 of 88,756 hypertensive adults found the risk of CV event or death increased with delay of medication intensification from the lowest delay (0 – 1.4 months) to the highest delay (4.7 months) (HR 1.12, 95% CI [1.05 – 1.20], p=0.009).
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.
- Egan BM, Bandyopadhyay D, Shaftman SR, Wagner CS, Zhao Y, Yu-Isenberg KS. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension 2012; 59 (6): 1124-1131.
- Gradman AH, Parise H, Lefebvre P, Falvey H, Lafeuille MH, Duh MS. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension 2013; 61 (2): 309-318.
- Corrao G, Nicotra F, Parodi A, et al. Cardiovascular protection by initial and subsequent combination of antihypertensive drugs in daily life practice. Hypertension 2011; 58 (4): 566-572.
- Xu W, Goldberg SI, Shubina M, Turchin A. Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study. BMJ 2015; 350: h158.

.png)