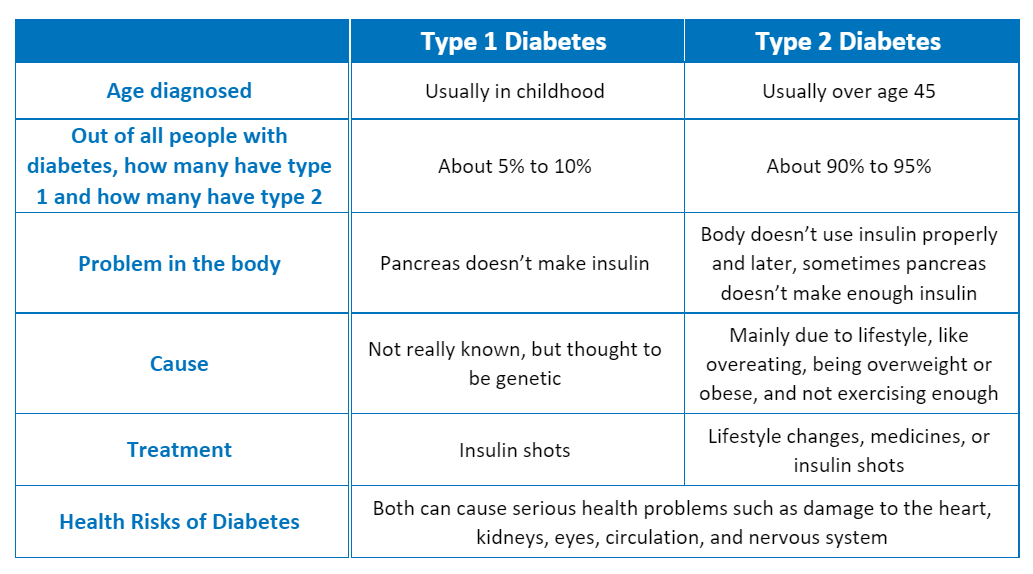
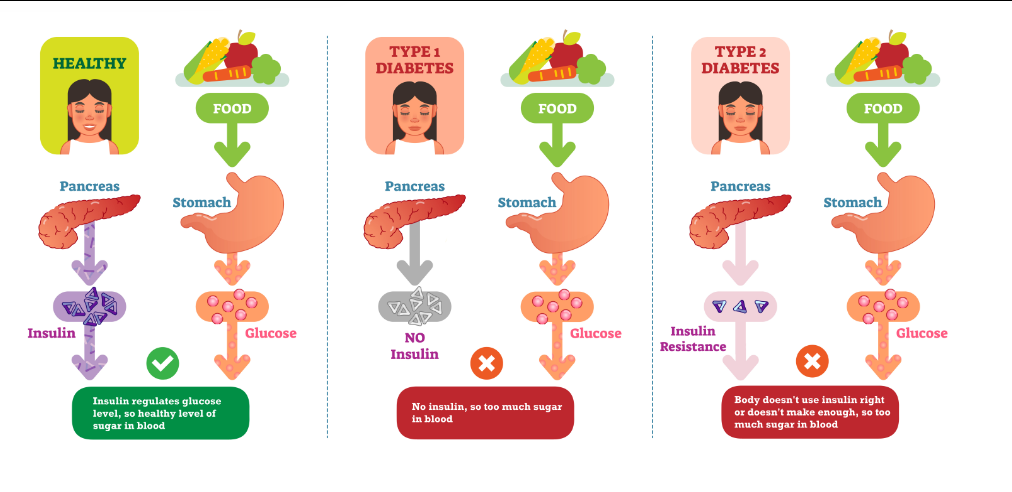
Diabetes is a chronic condition of high blood glucose levels due to low or no levels of insulin, insulin resistance, or both.1-3 Insulin resistance occurs when cells in the muscles, fat, and liver don't respond appropriately to insulin, decreasing glucose uptake from the blood, resulting in high blood sugar levels.4 Diabetes is divided into two types with differing disease progressions and treatments.
Type 1 diabetes is a genetic condition usually diagnosed early in life characterized by autoimmune or idiopathic destruction of insulin-producing β-cells in the pancreas, which leads to complete insulin deficiency.2,3,5,6 Markers of β-cell immune destruction are present in 90% of people at diagnosis. Autoimmune markers include autoantibodies to insulin, GAD65, tyrosine phosphatases IA-2 and IA 2β, and islet cells.2,6,7 A minority of patients with type 1 diabetes have no evidence of β-cell autoimmunity although they still exhibit β-cell destruction, which is referred to as idiopathic type 1 diabetes. Further research is needed to determine the cause of β-cell destruction in these cases. Type 1 diabetes accounts for roughly 5-10% of all diabetes cases.
Type 2 diabetes, also called type 2 diabetes mellitus, is a condition of insulin resistance out of proportion to insulin production.2,8-10 It develops over the course of years based on environmental and lifestyle factors and results in the body either being unable to respond to insulin or unable to produce enough. Type 2 diabetes accounts for 90% to 95% of all diabetes.1,11 It typically develops in people over age 45 but can occur in younger adults and children.
Type 1 diabetes was previously known as juvenile-onset or insulin-dependent diabetes while type 2 diabetes was previously known as adult-onset or noninsulin-dependent diabetes. The idea that type 2 diabetes only develops in adults and type 1 diabetes only in children is no longer accurate as both diseases occur in both age groups, though type 1 diabetes is more likely to be diagnosed at a young age than adulthood. Similarly, both type 1 and type 2 diabetes can be insulin dependent, although all type 1 diabetics are insulin dependent.2,5
Risk Factors
The risk factors for developing type 1 diabetes are largely unknown, however there is increasing evidence for genetic, environmental, or viral factors playing a role in the development of both autoimmune and idiopathic type 1 diabetes.2,12,13
The risk factors for developing type 2 diabetes include:
- Older age
- Overweight or obesity
- Lack of physical activity
- Prior diabetes while pregnant (gestational diabetes)
- High blood pressure
- High lipid levels
- Polycystic ovary syndrome
- Certain medications including some HIV medications, glucocorticoids, thiazide diuretics, and atypical antipsychotics.
- Family history of type 2 diabetes in a first degree relative
- Certain racial and ethnic groups including blacks, Native Americans, Asians, Hispanics, and Latinos
Symptoms
Type 1 and type 2 diabetes share common symptoms, although symptoms tend to be more acute and come on more quickly for patients with type 1 diabetes. Symptoms include:
- Increased thirst
- Increased urination
- Fatigue
- Excessive hunger
- Blurry vision
- Irritability and mood changes
- Unexpected weight loss
- Cuts, sores, and bruises that heal slowly
Diagnosis
Type 1 and type 2 diabetes have the same diagnostic criterion, which include any of the following:
- Fasting plasma glucose levels ≥125 mg/dL
- 2-hour plasma glucose levels ≥200 mg/dL during oral glucose tolerance test
- Glycated hemoglobin (A1C) of greater than or equal to 6.5%
- In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL
Patients diagnosed with type 1 diabetes are typically highly symptomatic. Some may present with diabetic ketoacidosis (DKA) as the first manifestation of the disease. Others have modest fasting hyperglycemia that can rapidly change to severe hyperglycemia. Conversely, most people with type 2 diabetes don’t have any symptoms at first and are identified with screening tests.1,11
Treatment
Patients with type 1 diabetes are insulin dependent. This means they require insulin injections as treatment. Patients with type 2 diabetes are not typically dependent on insulin for treatment at diagnosis. Treatments for type 2 diabetes can include lifestyle changes, various oral medications, and for severe cases, insulin injections.
Health Risks
Without treatment, people with all types of diabetes have a much higher risk of complications such as:1,5,14
- Hyperglycemic and hypoglycemic crises requiring emergency help or hospital treatment
- Cardiovascular disease (heart attack, stroke, ischemic heart disease)
- Kidney disease and failure
- Vision loss and blindness
- Neurological disease
- Sexual dysfunction
- Dental problems
- Foot ulcers and amputations
References
- Vijan S. Type 2 diabetes. Ann Intern Med. Nov 5 2019;171(9):Itc65-itc80. doi:10.7326/aitc201911050
- Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes care. Jan 2020;43(Suppl 1):S14-s31. doi:10.2337/dc20-S002
- Thomas NJ, Lynam AL, Hill AV, et al. Type 1 diabetes defined by severe insulin deficiency occurs after 30 years of age and is commonly treated as type 2 diabetes. Diabetologia. Jul 2019;62(7):1167-1172. doi:10.1007/s00125-019-4863-8
- Diseases NIoDaDaK. Insulin Resistance & Prediabetes. 2022. Accessed 2022, https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance#:~:text=the%20normal%20range.-,What%20is%20insulin%20resistance%3F,help%20glucose%20enter%20your%20cells.
- National Institute of Diabetes and Digestive and Kidney Diseases. What is diabetes? NIH. Accessed January 16, 2020. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
- 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes care. 2021;44(Supplement 1):S15-S33. doi:10.2337/dc21-S002
- Solis-Herrera C TC, Reasner C. Classification of Diabetes Mellitus. In: Feingold KR AB, Boyce A, ed. Endotext [Internet]. MDText.com, Inc; 2018. https://www.ncbi.nlm.nih.gov/books/NBK279119/
- Beck-Nielsen H, Groop LC. Metabolic and genetic characterization of prediabetic states. Sequence of events leading to non-insulin-dependent diabetes mellitus. The Journal of clinical investigation. Nov 1994;94(5):1714-21. doi:10.1172/jci117518
- Kahn CR. Banting Lecture. Insulin action, diabetogenes, and the cause of type II diabetes. Diabetes. Aug 1994;43(8):1066-84. doi:10.2337/diab.43.8.1066
- Robertson RP. Antagonist: diabetes and insulin resistance--philosophy, science, and the multiplier hypothesis. The Journal of laboratory and clinical medicine. May 1995;125(5):560-4; discussion 565.
- 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes care. Jan 2021;44(Suppl 1):S15-s33. doi:10.2337/dc21-S002
- Thomas NJ, Jones SE, Weedon MN, Shields BM, Oram RA, Hattersley AT. Frequency and phenotype of type 1 diabetes in the first six decades of life: a cross-sectional, genetically stratified survival analysis from UK Biobank. Lancet Diabetes Endocrinol. Feb 2018;6(2):122-129. doi:10.1016/s2213-8587(17)30362-5
- Filippi CM, von Herrath MG. Viral trigger for type 1 diabetes: pros and cons. Diabetes. Nov 2008;57(11):2863-71. doi:10.2337/db07-1023
- National Diabetes Statistics Report (Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services) (2020).
.png)
