Hyperlipidemia or dyslipidemia, generalized as high cholesterol, is characterized by elevated blood serum levels of low-density lipoprotein (LDL) and triglycerides and low levels of high-density lipoprotein (HDL).1 All of these measurements together are known as total cholesterol (TC).
Table 1. Recommended cholesterol levels for otherwise healthy adults presented in mg/dL1,2
|
LDL
|
|
Ideal
|
<100
|
|
Near optimal
|
100-129
|
|
Borderline high
|
130-159
|
|
High
|
160-189
|
|
Severe
|
≥190
|
|
Triglycerides
|
|
Ideal
|
<150
|
|
Borderline high
|
150-199
|
|
High
|
200-499
|
|
Severe
|
≥500
|
|
TC
|
|
Ideal
|
<200
|
|
Borderline high
|
200-239
|
|
High
|
≥240
|
There are several causes of hyperlipidemia, including heritable traits (e.g., familial dyslipidemia3), lifestyle factors (e.g., diet,4 obesity,5 smoking6), medical conditions, and medications. High cholesterol has been cited as a sequela of several diseases such as diabetes,7 hypothyroidism,8 chronic kidney disease,9 liver disease,10 HIV/AIDS11, and lupus.12 Medications such as amiodarone,13 beta blockers,14 loop and thiazide diuretics,15 hormones,16,17 androgen steroids,18 corticosteroids,19 antipsychotics,20,21 immunosuppressants,22 antivirals,23 and retinoids24 have also been linked to higher levels of cholesterol.
According to American College of Cardiology/American Heart Association (ACC/AHA) guidelines, the first and strongest recommended therapeutic modality is lifestyle therapies25, including modifications to diet composition, weight control, and physical activity.1
Diet
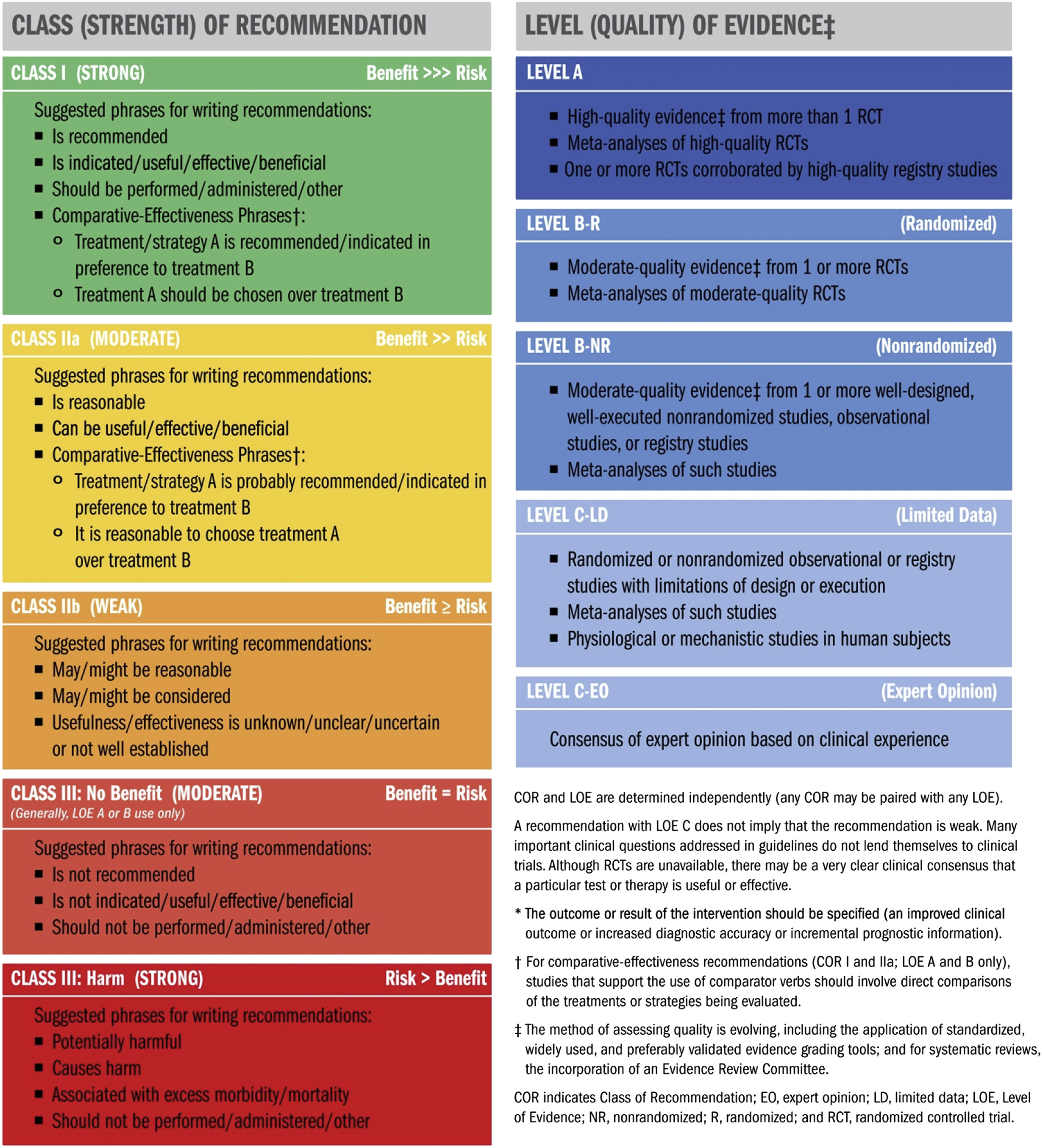
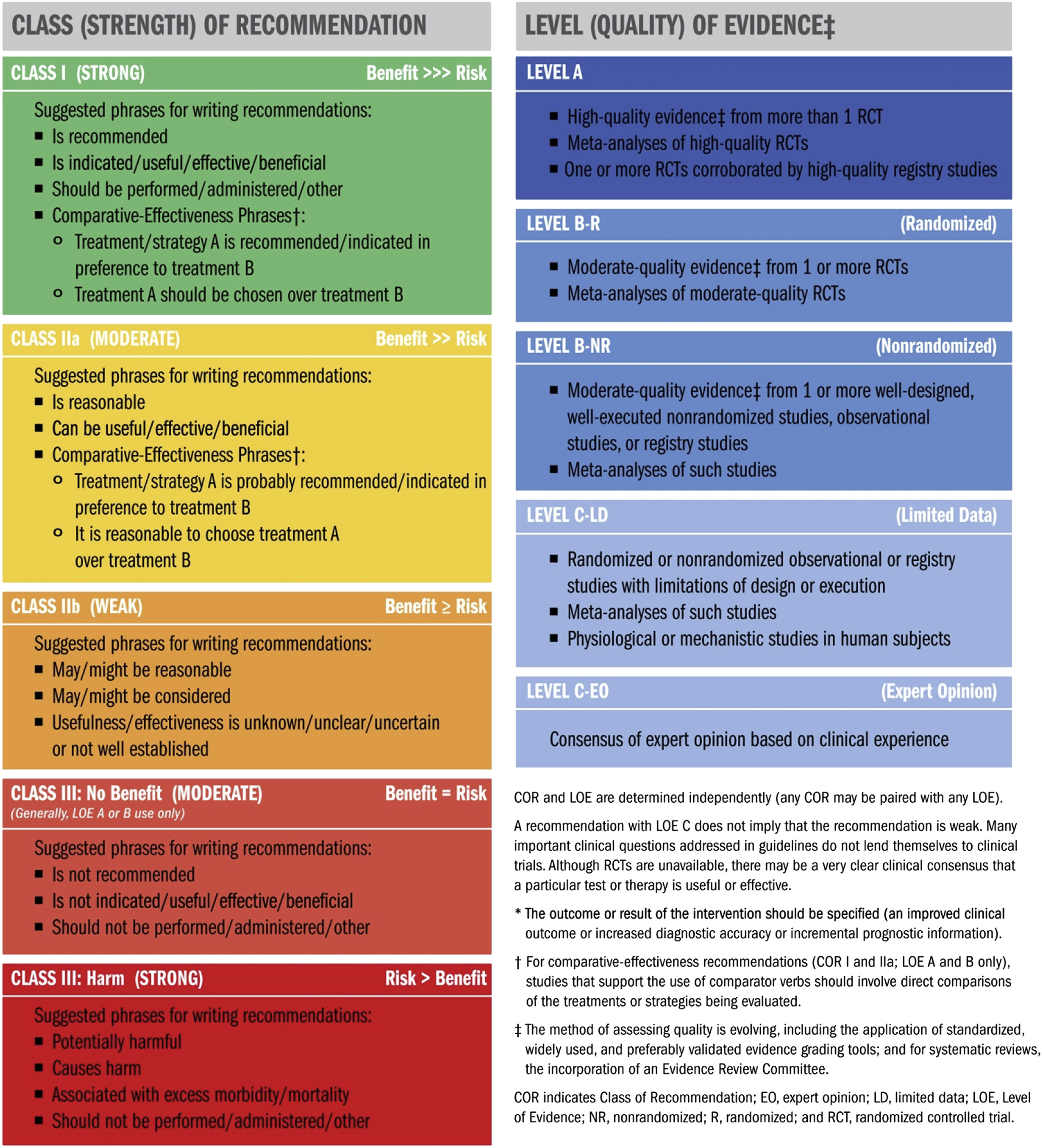
The ACC/AHA recommends that patients follow a healthy eating pattern, encouraging intake of vegetables, fruits, whole grains, legumes, healthy protein sources, and non-tropical vegetable oils while limiting intake of sweets, sugar-sweetened beverages, and red meats (Class of Recommendation [COR] I, Level of Evidence [LOE] A).*4 This recommendation is based largely on studies of the Dietary Approaches to Stop Hypertension (DASH) diet and its variations. According to the ACC/AHA analysis of these studies, they have shown that compared to a typical American diet, the DASH diet lowered LDL by about 11 mg/dL while having no effect on triglycerides. This LDL lowering effect was found in adults of all ages and among men, women, African Americans, non-African Americans, hypertensive, and normotensive adults.
Similarly, slight variations on the DASH diet, such as replacing 10% of calories from carbohydrates with protein, also lowered LDL, but more moderately, by about 3 mg/dL, and had a greater effect on triglycerides, lowering by about 16 mg/dL.4 Replacing 10% of calories from carbohydrates with unsaturated fat lowered LDL similarly by 3 mg/dL but lowered triglycerides by 10 mg/dL.
They also recommend aiming to only consume 5-6% of daily caloric intake from saturated fat and to reduce intake of saturated and trans-fat in general (COR I, LOE A).4 Based on their analysis of studies examining the effect of dietary fat on cholesterol, they found that when adults consumed only 5-6% of their daily caloric intake from saturated fat compared to a control group consuming 14-15% saturated fat, LDL was lowered by about 11-13 mg/dL. In controlled feeding trials, for every 1% of energy from saturated fatty acids (SFA) or trans fats that is replaced by carbohydrates, monounsaturated fatty acids (MUFA), or polyunsaturated fatty acids (PUFA), they found that LDL is lowered.
Table 1. Decrease in serum cholesterol per each 1% of total caloric intake of SFA, carbohydrates, or trans fats replaced with PUFA, MUFA, or carbohydrates (all presented in mg/dL).4
|
|
PUFA
|
MUFA
|
Carbohydrates
|
|
Replacing SFA
|
|
LDL
|
1.8
|
1.3
|
1.2
|
|
Triglycerides
|
0.4
|
N/A (Raised by 0.2)
|
N/A (Raised by 1.9)
|
|
Replacing carbohydrate
|
|
LDL
|
0.7
|
0.3
|
|
|
Triglycerides
|
2.3
|
1.7
|
|
|
Replacing trans fats
|
|
LDL
|
2.0
|
1.5
|
1.5
|
|
Triglycerides
|
1.3
|
1.2
|
N/A (No effect)
|
The relationship between diets high in dietary cholesterol and subsequent high cholesterol levels is unclear.4 Some studies have shown a positive correlative relationship, but many don’t account for the fact that foods high in cholesterol content are also rich in SFA. A 2012-2016 Korea National Health and Nutrition Examination Survey (KNHANES) study that included 39,156 participants found no significant associations between dietary cholesterol intake and TC or LDL levels after controlling for saturated fat intake.26
While high dietary cholesterol alone does not appear to contribute to hypercholesterolemia, because most foods high in cholesterol are more caloric and contain more fat, a diet high in cholesterol can contribute to hyperlipidemia. Additionally, because of cholesterol’s relationship with higher overall calorie and fat intake, diets high in cholesterol can lead to obesity, another secondary cause of hyperlipidemia.5
Exercise
A prospective study (n=27,055) of otherwise healthy women estimated that the beneficial effects of physical activity on serum lipid levels accounted for 19% of the observed reduction in cardiovascular disease risk.27
For adults, the ACC/AHA recommends three to four 40-minute sessions of aerobic physical activity each week to reduce LDL and other non-HDL cholesterol (CoR IIa, LoE A).4 In studies of physical activity not in combination with any other intervention, aerobic physical activity has been found to reduce LDL by 3-6 mg/dL on average.
Long Term Effects of High Cholesterol
High cholesterol is a risk factor for the development of atherosclerotic cardiovascular disease (ASCVD).1 Cholesterol contributes to ASCVD progression when the accumulation of cholesterol particles in blood vessel walls causes decreased blood flow through the vessel.
*See ACC/AHA Class of Recommendation and Level of Evidence definitions below:
References
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. Jun 25 2019;73(24):e285-e350. doi:10.1016/j.jacc.2018.11.003
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. Dec 17 2002;106(25):3143-421.
- Hopkins PN, Toth PP, Ballantyne CM, Rader DJ. Familial hypercholesterolemias: prevalence, genetics, diagnosis and screening recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol. Jun 2011;5(3 Suppl):S9-17. doi:10.1016/j.jacl.2011.03.452
- Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. Jun 24 2014;129(25 Suppl 2):S76-99. doi:10.1161/01.cir.0000437740.48606.d1
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. Jun 24 2014;129(25 Suppl 2):S102-38. doi:10.1161/01.cir.0000437739.71477.ee
- Forey BA, Fry JS, Lee PN, Thornton AJ, Coombs KJ. The effect of quitting smoking on HDL-cholesterol - a review based on within-subject changes. Biomark Res. Sep 13 2013;1(1):26. doi:10.1186/2050-7771-1-26
- Howard BV. Lipoprotein metabolism in diabetes mellitus. J Lipid Res. Jun 1987;28(6):613-28.
- Thompson GR, Soutar AK, Spengel FA, Jadhav A, Gavigan SJ, Myant NB. Defects of receptor-mediated low density lipoprotein catabolism in homozygous familial hypercholesterolemia and hypothyroidism in vivo. Proc Natl Acad Sci U S A. Apr 1981;78(4):2591-5. doi:10.1073/pnas.78.4.2591
- KDIGO Clinical Practice Guideline for Lipid Management in Chronic Kidney Disease. Kidney International Supplements. 2013;3(3):259-305.
- Harry DS, Day RC, Owen JS, Agorastos J, Foo AY, McIntyre N. Plasma lecithin:cholesterol acyltransferase activity and the lipoprotein abnormalities of liver disease. Scand J Clin Lab Invest Suppl. 1978;150:223-7. doi:10.3109/00365517809104930
- Friis-Møller N, Weber R, Reiss P, et al. Cardiovascular disease risk factors in HIV patients--association with antiretroviral therapy. Results from the DAD study. Aids. May 23 2003;17(8):1179-93. doi:10.1097/01.aids.0000060358.78202.c1
- Urowitz MB, Gladman D, Ibañez D, et al. Clinical manifestations and coronary artery disease risk factors at diagnosis of systemic lupus erythematosus: data from an international inception cohort. Lupus. 2007;16(9):731-5. doi:10.1177/0961203307081113
- Albert SG, Alves LE, Rose EP. Thyroid dysfunction during chronic amiodarone therapy. J Am Coll Cardiol. Jan 1987;9(1):175-83. doi:10.1016/s0735-1097(87)80098-0
- Day JL, Simpson N, Metcalfe J, Page RL. Metabolic consequences of atenolol and propranolol in treatment of essential hypertension. Br Med J. Jan 13 1979;1(6156):77-80. doi:10.1136/bmj.1.6156.77
- McKenney JM, Goodman RP, Wright JT, Jr., Rifai N, Aycock DG, King ME. The effect of low-dose hydrochlorothiazide on blood pressure, serum potassium, and lipoproteins. Pharmacotherapy. Jul-Aug 1986;6(4):179-84. doi:10.1002/j.1875-9114.1986.tb03473.x
- Wahl P, Walden C, Knopp R, et al. Effect of estrogen/progestin potency on lipid/lipoprotein cholesterol. N Engl J Med. Apr 14 1983;308(15):862-7. doi:10.1056/nejm198304143081502
- Birjmohun RS, Kees Hovingh G, Stroes ES, et al. Effects of short-term and long-term danazol treatment on lipoproteins, coagulation, and progression of atherosclerosis: two clinical trials in healthy volunteers and patients with hereditary angioedema. Clin Ther. Dec 2008;30(12):2314-23. doi:10.1016/j.clinthera.2008.12.021
- McKillop G, Ballantyne D. Lipoprotein analysis in bodybuilders. Int J Cardiol. Dec 1987;17(3):281-8. doi:10.1016/0167-5273(87)90077-5
- Zimmerman J, Fainaru M, Eisenberg S. The effects of prednisone therapy on plasma lipoproteins and apolipoproteins: a prospective study. Metabolism. Jun 1984;33(6):521-6. doi:10.1016/0026-0495(84)90006-4
- Gaulin BD, Markowitz JS, Caley CF, Nesbitt LA, Dufresne RL. Clozapine-associated elevation in serum triglycerides. Am J Psychiatry. Aug 1999;156(8):1270-2. doi:10.1176/ajp.156.8.1270
- Sasaki J, Kumagae G, Sata T, Kuramitsu M, Arakawa K. Decreased concentration of high density lipoprotein cholesterol in schizophrenic patients treated with phenothiazines. Atherosclerosis. May-Jun 1984;51(2-3):163-9. doi:10.1016/0021-9150(84)90164-3
- Ballantyne CM, Podet EJ, Patsch WP, et al. Effects of cyclosporine therapy on plasma lipoprotein levels. Jama. Jul 7 1989;262(1):53-6.
- Heath KV, Hogg RS, Chan KJ, et al. Lipodystrophy-associated morphological, cholesterol and triglyceride abnormalities in a population-based HIV/AIDS treatment database. Aids. Jan 26 2001;15(2):231-9. doi:10.1097/00002030-200101260-00013
- Bershad S, Rubinstein A, Paterniti JR, et al. Changes in plasma lipids and lipoproteins during isotretinoin therapy for acne. N Engl J Med. Oct 17 1985;313(16):981-5. doi:10.1056/nejm198510173131604
- Reddy KR. Cardiovascular Disease and Lifestyle Medicine. J Fam Pract. Jan 2022;71(Suppl 1 Lifestyle):S48-s55. doi:10.12788/jfp.0251
- Cha D, Park Y. Association between Dietary Cholesterol and Their Food Sources and Risk for Hypercholesterolemia: The 2012⁻2016 Korea National Health and Nutrition Examination Survey. Nutrients. Apr 15 2019;11(4)doi:10.3390/nu11040846
- Mora S, Cook N, Buring JE, Ridker PM, Lee IM. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. Nov 6 2007;116(19):2110-8. doi:10.1161/circulationaha.107.729939