Lupus is a chronic, inflammatory autoimmune disease that can affect almost any organ in the body. Clinical presentations are heterogenous and range from mild to life-threatening.1
Constitutional symptoms
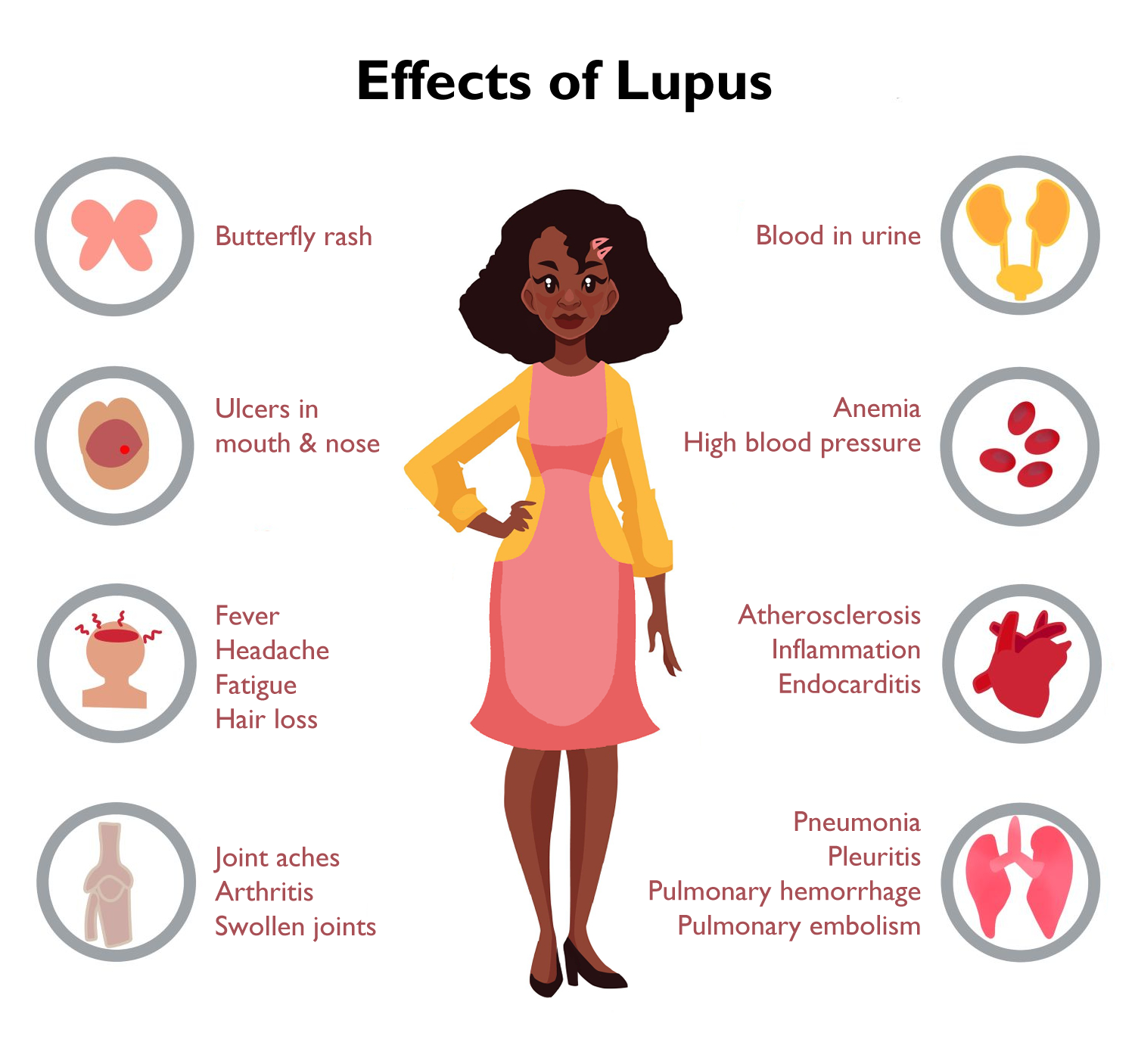
Constitutional symptoms are common in patients with lupus and include fatigue, fever, myalgias, and weight changes. These systemic symptoms may affect patients at any point in the course of the disease. Fatigue is one of the most common symptoms at presentation, occurring in 80 to 100 percent of patients who are diagnosed with lupus.2 The intensity of fatigue may be significant and has been found to correlate with concomitant mood disorders and insomnia, though it has no clear relationship with disease severity.2 Fever is a common but nonspecific sign of active disease and occurs in approximately 50 percent of lupus patients.3 Clinical context is important to the finding of fever in a patient with lupus. These patients are at higher risk of infection due to frequent treatment with and other immunosuppressive medications, so fever may be a sign of active infection rather than underlying disease.4 Both weight gain and loss are commonly connected to lupus. Unintentional weight loss often occurs prior to disease but can also occur later in the disease course due to medication adverse effects or increased disease activity. Weight gain may occur due to medication adverse effects (e.g., corticosteroid use) or in the setting of nephrotic syndrome.1,3
Musculoskeletal symptoms
Joint involvement is present in nearly all patients with lupus. Studies demonstrates that nearly 90 percent of lupus patients experience arthritis or arthralgias, which often occur early in the disease course.3,5 Often, joint pain is the leading complaint that causes patients to seek medical care prior to diagnosis.1 Joint involvement in lupus has a heterogenous presentation, ranging from mild to severe arthritis, and can involve one joint or multiple joints.6 Arthritis caused by lupus is typically symmetrical, migratory, characterized by morning stiffness, and most commonly affects the hands and wrists.7 There is evidence of significant inflammation in about 70 percent of patients, but lupus-associated joint inflammation is rarely erosive or deforming, except in severe cases which may appear more similar to rheumatoid arthritis.7
Mucocutaneous manifestations
Mucocutaneous manifestations occur in most patients with lupus and have phenotypic heterogeneity.8 About 80 percent of lupus patients experience cutaneous manifestations, and nearly 25 percent of patients have a cutaneous manifestation as the first sign of disease.9 Acute cutaneous lupus erythema is the classic cutaneous manifestation and is colloquially known as “the butterfly rash.” It presents as an erythematous, malar rash across the nose and cheeks, sparing the nasolabial folds. A 10-year cohort study following patients with lupus found that 31% of patients experienced acute cutaneous lupus erythema at least once during that period.3 Skin photosensitivity, inflammatory discoid lesions, and painless ulcers in the mouth or nose are other common mucocutaneous manifestations of lupus.9
Renal involvement
Renal disease or lupus nephritis affects approximately 50% of patients with lupus. Of those patients with lupus nephritis, approximately 15% develop advanced renal disease, defined as end-stage renal disease, and may require dialysis and eventually a kidney transplant.3,10 Patients may present with asymptomatic hematuria or proteinuria, clinically evident nephrotic syndrome, or rapidly progressive renal failure. In clinically asymptomatic cases, lupus nephritis is often only detected via routine screening with renal function laboratory tests and urinalysis. Periodic screenings are critical for the early detection and treatment of lupus nephritis to prevent renal damage.11
Neurologic and Psychiatric involvement
Neurologic and psychiatric involvement in lupus is widely heterogenous. Neuropsychiatric manifestations are difficult to assess due to the inherent complexities of diagnosis; the symptoms may be a direct consequence of lupus itself, due to comorbid conditions, complications of treatment, unrelated etiologies, or a combination of these factors. An international cohort study following 1,206 patients with lupus found that 40 percent experienced a neuropsychiatric event over a period of three years.12 Neuropsychiatric manifestations of lupus include stroke, seizures, peripheral neuropathies, movement disorders, cognitive impairment, psychosis, delirium, and, less commonly, myelitis and meningitis.1,3 These occur most commonly around the time of initial diagnosis but can develop at any point in the disease course. Although many neuropsychiatric events completely resolve, some may cause persistent symptoms. Neuropsychiatric involvement in lupus is associated with reduced quality of life and increased mortality.12
Cardiovascular involvement
Cardiac involvement commonly affects the pericardium. It causes pericarditis, with or without effusion, in approximately 25 percent of patients with lupus.13 The myocardium, valves, and conduction system may also be affected in lupus.13,14 Cardiovascular involvement further includes coronary heart disease, which is when blood flow to the heart is limited due to narrowing of its major blood vessels, usually due to the buildup of plaque. Coronary heart disease is responsible for significant morbidity and mortality in this population.15 A systematic review of 28 studies found that the risk of atherosclerotic cardiovascular disease (e.g., cerebrovascular accidents, coronary artery disease, myocardial infarction, and peripheral vascular disease) in people with lupus is doubled relative to the general population.16 The increased relative risk is particularly high among young women with lupus, given the relatively low risk of heart disease among their counterparts in the general population. For example, a prospective cohort from the Nurses’ Health Study found that among women with lupus compared to the general population, the relative risk for coronary heart disease was 2.25 (95% confidence interval [1.37 – 3.69]).17 Though the magnitude of increased relative risk varies between different epidemiologic studies, the overall finding that lupus patients have an increased risk of cardiovascular disease is supported by robust and well-replicated evidence. 16, 18
Pulmonary involvement
Pulmonary involvement in lupus can affect all structures of the lungs, pleura, and pulmonary vasculature.19 The most common pulmonary manifestation is pleuritis, which affects approximately 50% of patients with lupus.20 Lupus can also cause interstitial lung disease (estimated prevalence 3 to 8%), lupus pneumonitis (1 to 4%), alveolar hemorrhage (0.5%), pulmonary hypertension (5%), and shrinking lung syndrome (0.5%).14,20 Patients with antiphospholipid antibodies are at higher risk of pulmonary embolism.19 Clinically, patients often present with dyspnea, pleurisy, and coughing. Respiratory infection is an important alternative etiology to consider in these presentations, especially in patients with active or recent treatment with immunosuppressive medications.
Antiphospholipid syndrome
Antiphospholipid syndrome (APS) is a multisystem autoimmune disease that is associated with lupus and is characterized by thromboembolic events and pregnancy complications in the presence of antiphospholipid antibodies.21 Of all patients with lupus, 30 to 40 percent have antiphospholipid antibodies22 and 10 to 25 percent have APS.21,23 The clinical manifestations of APS are widespread and include venous and arterial thrombosis, thrombocytopenia, cardiac valve thickening or nodules (e.g. Libman-Sacks endocarditis), stroke, transient ischemic attack, pulmonary embolism, and pregnancy complications, such as fetal loss.21
References :
- Kiriakidou M, Ching CL. Systemic Lupus Erythematosus. Ann Intern Med. 2020;172(11):ITC81-ITC96. doi:10.7326/AITC202006020
- Tench CM, McCurdie I, White PD, D'Cruz DP. The prevalence and associations of fatigue in systemic lupus erythematosus. Rheumatology (Oxford). 2000;39(11):1249-1254. doi:10.1093/rheumatology/39.11.1249
- Cervera R, Khamashta MA, Font J, et al. Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients. Medicine (Baltimore). 2003;82(5):299-308. doi:10.1097/01.md.0000091181.93122.55
- Rovin BH, Tang Y, Sun J, et al. Clinical significance of fever in the systemic lupus erythematosus patient receiving steroid therapy. Kidney Int. 2005;68(2):747-759. doi:10.1111/j.1523-1755.2005.00453.x
- Greco CM, Rudy TE, Manzi S. Adaptation to chronic pain in systemic lupus erythematosus: applicability of the multidimensional pain inventory. Pain Med. 2003;4(1):39-50. doi:10.1046/j.1526-4637.2003.03001.x
- Gormezano NW, Silva CA, Aikawa NE, et al. Chronic arthritis in systemic lupus erythematosus: distinct features in 336 paediatric and 1830 adult patients. Clin Rheumatol. 2016;35(1):227-231. doi:10.1007/s10067-015-3127-3
- Ceccarelli F, Perricone C, Cipriano E, et al. Joint involvement in systemic lupus erythematosus: From pathogenesis to clinical assessment. Semin Arthritis Rheum. 2017;47(1):53-64. doi:10.1016/j.semarthrit.2017.03.022
- Ribero S, Sciascia S, Borradori L, Lipsker D. The Cutaneous Spectrum of Lupus Erythematosus. Clin Rev Allergy Immunol. 2017;53(3):291-305. doi:10.1007/s12016-017-8627-2
- Rothfield N, Sontheimer RD, Bernstein M. Lupus erythematosus: systemic and cutaneous manifestations. Clin Dermatol. 2006;24(5):348-362. doi:10.1016/j.clindermatol.2006.07.014
- Tektonidou MG, Dasgupta A, Ward MM. Risk of End-Stage Renal Disease in Patients With Lupus Nephritis, 1971-2015: A Systematic Review and Bayesian Meta-Analysis. Arthritis Rheumatol. 2016;68(6):1432-1441. doi:10.1002/art.39594
- Danila MI, Pons-Estel GJ, Zhang J, Vilá LM, Reveille JD, Alarcón GS. Renal damage is the most important predictor of mortality within the damage index: data from LUMINA LXIV, a multiethnic US cohort. Rheumatology (Oxford). 2009;48(5):542-545. doi:10.1093/rheumatology/kep012
- Hanly JG, Urowitz MB, Su L, et al. Prospective analysis of neuropsychiatric events in an international disease inception cohort of patients with systemic lupus erythematosus. Ann Rheum Dis. 2010;69(3):529-535. doi:10.1136/ard.2008.106351
- Miner JJ, Kim AH. Cardiac manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. 2014;40(1):51-60. doi:10.1016/j.rdc.2013.10.003
- Tselios K, Urowitz MB. Cardiovascular and Pulmonary Manifestations of Systemic Lupus Erythematosus. Curr Rheumatol Rev. 2017;13(3):206-218. doi:10.2174/1573397113666170704102444
- Lisnevskaia L, Murphy G, Isenberg D. Systemic lupus erythematosus. Lancet. 2014;384(9957):1878-1888. doi:10.1016/S0140-6736(14)60128-8
- Schoenfeld SR, Kasturi S, Costenbader KH. The epidemiology of atherosclerotic cardiovascular disease among patients with SLE: a systematic review. Semin Arthritis Rheum. 2013;43(1):77-95. doi:10.1016/j.semarthrit.2012.12.002
- Hak AE, Karlson EW, Feskanich D, Stampfer MJ, Costenbader KH. Systemic lupus erythematosus and the risk of cardiovascular disease: results from the nurses' health study. Arthritis Rheum. 2009;61(10):1396-1402.
- Symmons DP, Gabriel SE. Epidemiology of CVD in rheumatic disease, with a focus on RA and SLE. Nat Rev Rheumatol. 2011;7(7):399-408. Published 2011 May 31. doi:10.1038/nrrheum.2011.75
- Keane MP, Lynch JP 3rd. Pleuropulmonary manifestations of systemic lupus erythematosus. Thorax. 2000;55(2):159-166. doi:10.1136/thorax.55.2.159
- Torre, O., & Harari, S. (2011). Pleural and pulmonary involvement in systemic lupus erythematosus. Presse medicale (Paris, France : 1983), 40(1 Pt 2), e19–e29. https://doi.org/10.1016/j.lpm.2010.11.004
- Schreiber K, Sciascia S, de Groot PG, et al. Antiphospholipid syndrome [published correction appears in Nat Rev Dis Primers. 2018 Jan 25;4:18005]. Nat Rev Dis Primers. 2018;4:17103. Published 2018 Jan 11. doi:10.1038/nrdp.2017.103
- Abu-Shakra M, Gladman DD, Urowitz MB, Farewell V. Anticardiolipin antibodies in systemic lupus erythematosus: clinical and laboratory correlations. Am J Med. 1995;99(6):624-628. doi:10.1016/s0002-9343(99)80249-6
- Franco JS, Molano-González N, Rodríguez-Jiménez M, et al. The coexistence of antiphospholipid syndrome and systemic lupus erythematosus in Colombians. PLoS One. 2014;9(10):e110242. Published 2014 Oct 24. doi:10.1371/journal.pone.0110242