Observational studies have demonstrated that total cholesterol is associated with ischemic heart disease and stroke rates and that this relationship is continuous as blood concentrations of cholesterol increase.1 A cholesterol screening is one of the first courses of action to determine a patient’s risk for cardiovascular disease (CVD) events and create a care plan. The American College of Cardiology and the American Heart Association (ACC/AHA) guideline recommends cardiovascular disease (CVD) risk screening, including cholesterol testing, every 4-6 years for otherwise healthy adults.2 People with increased risk factors for CVD should get their cholesterol tested more often based on their 10-year CVD risk score – the higher an individual’s risk, the more often they should be tested at the discretion of their healthcare provider.
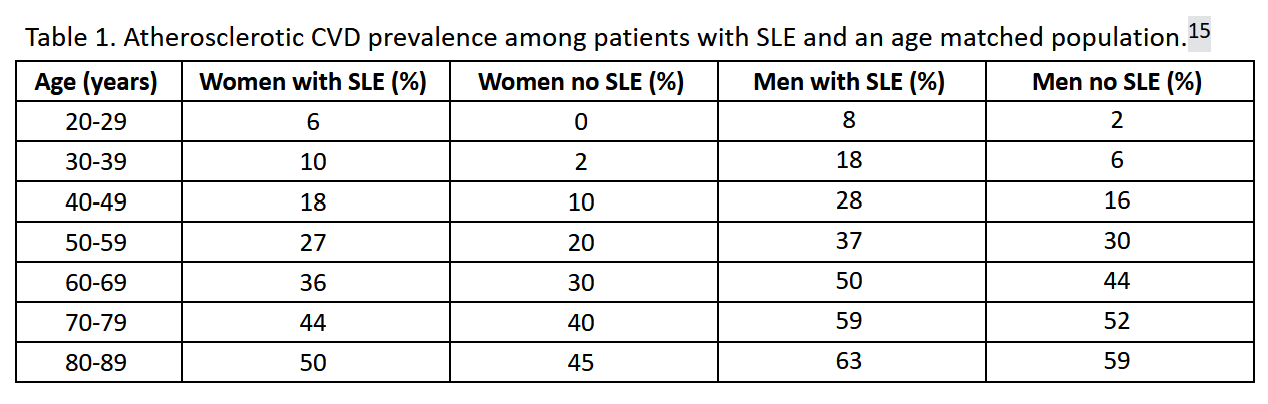
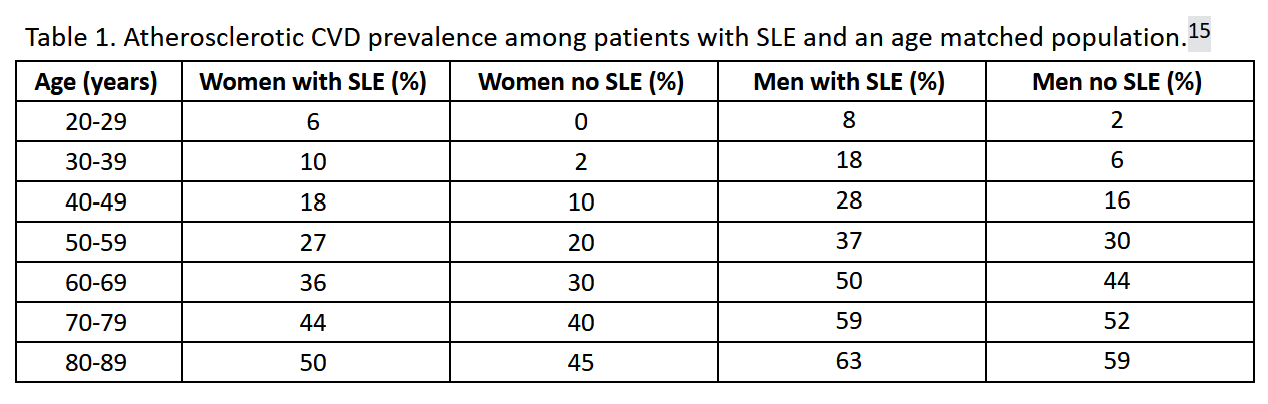
Compared to the general population, people diagnosed with systemic lupus erythematosus (SLE), commonly referred to as lupus, have a higher risk of experiencing CVD events, including myocardial infarction (MI) and stroke, as well as CVD-related mortality.3-16 One study (n=1,010,710) found that over seven years, patients with SLE had a 6.4% higher prevalence of CVD compared with age and sex matched control patients (25.6% vs 19.2%)(odds ratio [OR] 1.45, 95% CI [1.44-1.47], p<0.001).15 A systematic review including 28 studies found that the relative risk of CVD in people with SLE was at least doubled compared to age-matched people without SLE.13
Younger patients have an even steeper increase in risk, especially for young women due to the relatively lower level of CVD rates as compared to the age matched population. One case-control study of adults (89% women) with (n=252,676) and without SLE (n=758,034) found that after multivariable adjustment, SLE was associated with increased atherosclerotic CVD prevalence, which was observed in both sexes and was greatest in younger patients (adjusted OR 1.46. 95% CI [1.41-1.51]).15
Another study looked at the incidence of CVD in patients with SLE (n=277) to age and sex matched controls without SLE (n=586) in northern Sweden over the course of 7 years.4 They also found that the most elevated risk of CVD and MI was seen among younger premenopausal women with SLE aged 40-49.4 Incidence rate (IR) of CVD in patients with SLE from age 40-49 was 8.00 (95% CI [1.65-23.38]) while overall IR for SLE patients was 1.27 (95% CI [0.82-1.87]). For MI, patients with SLE between 40-49 had an IR of 8.7 (95% CI [1.1-31.4]) while overall IR in women with SLE was 1.75 (95% CI [0.840-3.22]).4
A recent meta-analysis published in 2022 computed a pool estimate to determine the absolute risk and incidence rates of CVD events in adult patients with SLE using data from 46 studies.3 The absolute risk was 0.03 (95% CI [0.02-0.05]) for stroke (7 studies included), 0.01 (95% CI [0.00-0.02]) for MI (6 studies included), and 0.06 (95% CI [0.03-0.10]) for CVD factors (8 studies included). The pooled estimate for incidence rates of CVD events in patients with SLE per 1,000 persons per year was 4.72 for stroke (95% CI [3.35-6.32], 10 studies included), 2.81 for MI (95% CI [1.61-4.32], 6 studies included), and 11.21 for CVD factors (95% CI [8.48-14.32]).
The increase in CVD risk in patients with SLE is a leading cause of death among SLE patients.6,17 In a cohort study that followed 812 individuals with SLE for 10 years, 33% of deaths were caused by CVD events.18 A recent study which conducted a cause-of-death analysis on 1,593 deaths related to SLE found that when SLE was the underlying cause of death (n=637), the main non-underlying cause of death was CVD (49.5%). 17
The cause of increased CVD risk in patients with SLE is likely multifactorial. One systematic review article noted that elevated risks may be a combination of traditional risk factors (obesity, smoking, family history, etc.), inflammatory risk factors, and SLE-related risk factors (disease activity, disease duration, menopause, medication).13
While the ACC/AHA recommendation is that all individuals receive a cholesterol screening and cardiovascular risk assessment every 4-6 years, the European League Against Rheumatism (EULAR) guideline for CVD risk management recommends for patients with rheumatic and musculoskeletal diseases such as SLE to perform cholesterol screening within 6 months of diagnosis and repeat based on individual patient characteristics and risk levels.2,19 Further studies are needed to determine the optimal frequency of screening.
References
- Lewington S, Whitlock G, Clarke R, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet (London, England). 2007;370(9602):1829-1839.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563-e595.
- Bello N, Meyers KJ, Workman J, Hartley L, McMahon M. Cardiovascular events and risk in patients with systemic lupus erythematosus: Systematic literature review and meta-analysis. Lupus. 2022:9612033221147471.
- Bengtsson C, Ohman ML, Nived O, Rantapää Dahlqvist S. Cardiovascular event in systemic lupus erythematosus in northern Sweden: incidence and predictors in a 7-year follow-up study. Lupus. 2012;21(4):452-459.
- Bruce IN, Urowitz MB, Gladman DD, Hallett DC. Natural history of hypercholesterolemia in systemic lupus erythematosus. J Rheumatol. 1999;26(10):2137-2143.
- Elliott JR, Manzi S. Cardiovascular risk assessment and treatment in systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2009;23(4):481-494.
- Esdaile JM, Abrahamowicz M, Grodzicky T, et al. Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus. Arthritis Rheum. 2001;44(10):2331-2337.
- Jha SB, Rivera AP, Flores Monar GV, et al. Systemic Lupus Erythematosus and Cardiovascular Disease. Cureus. 2022;14(2):e22027.
- Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol. 1997;145(5):408-415.
- Manzi S, Selzer F, Sutton-Tyrrell K, et al. Prevalence and risk factors of carotid plaque in women with systemic lupus erythematosus. Arthritis Rheum. 1999;42(1):51-60.
- Petri M, Perez-Gutthann S, Spence D, Hochberg MC. Risk factors for coronary artery disease in patients with systemic lupus erythematosus. Am J Med. 1992;93(5):513-519.
- Petri M, Spence D, Bone LR, Hochberg MC. Coronary artery disease risk factors in the Johns Hopkins Lupus Cohort: prevalence, recognition by patients, and preventive practices. Medicine (Baltimore). 1992;71(5):291-302.
- Schoenfeld SR, Kasturi S, Costenbader KH. The epidemiology of atherosclerotic cardiovascular disease among patients with SLE: a systematic review. Semin Arthritis Rheum. 2013;43(1):77-95.
- Urowitz MB, Gladman D, Ibañez D, et al. Clinical manifestations and coronary artery disease risk factors at diagnosis of systemic lupus erythematosus: data from an international inception cohort. Lupus. 2007;16(9):731-735.
- Katz G, Smilowitz NR, Blazer A, Clancy R, Buyon JP, Berger JS. Systemic Lupus Erythematosus and Increased Prevalence of Atherosclerotic Cardiovascular Disease in Hospitalized Patients. Mayo Clin Proc. 2019;94(8):1436-1443.
- Roman MJ, Shanker BA, Davis A, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med. 2003;349(25):2399-2406.
- Thomas G, Mancini J, Jourde-Chiche N, et al. Mortality associated with systemic lupus erythematosus in France assessed by multiple-cause-of-death analysis. Arthritis Rheumatol. 2014;66(9):2503-2511.
- Bulkley BH, Roberts WC. The heart in systemic lupus erythematosus and the changes induced in it by corticosteroid therapy. A study of 36 necropsy patients. Am J Med. 1975;58(2):243-264.
- Drosos GC, Vedder D, Houben E, et al. EULAR recommendations for cardiovascular risk management in rheumatic and musculoskeletal diseases, including systemic lupus erythematosus and antiphospholipid syndrome. Ann Rheum Dis. 2022;81(6):768-779.