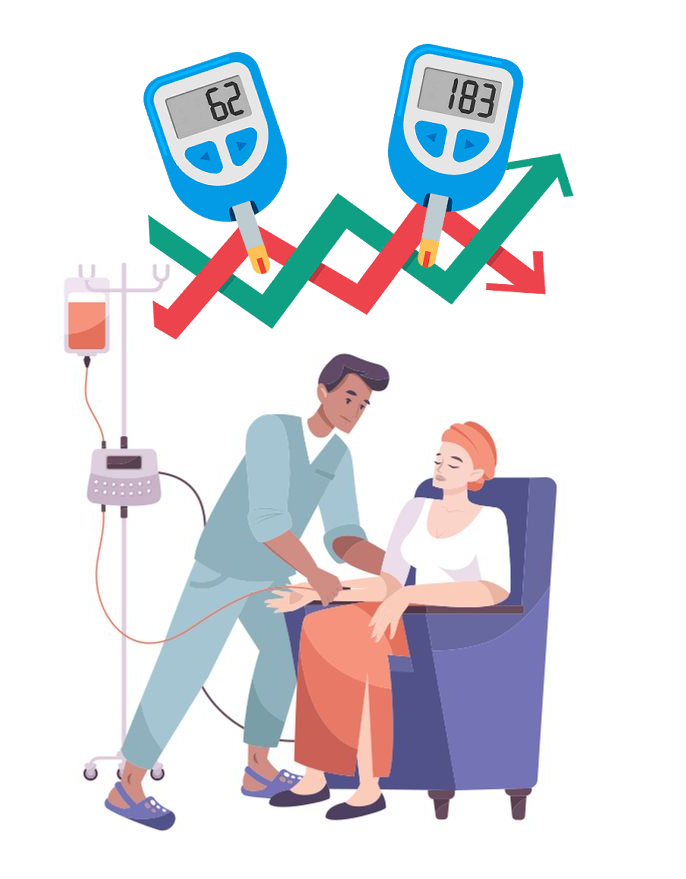
Cancer treatment can cause significant excursions in blood sugar, even in patients who normally achieve good glycemic control.1 Some chemotherapeutic regimens, such as corticosteroids, can raise blood glucose substantially. Chemotherapy is also accompanied by significant nausea in most patients, decreasing oral intake and potentially leading to dangerous levels of hypoglycemia if patients have taken full doses of oral diabetes medications or insulin and are then unable to eat.2,3 The profound fatigue that accompanies cancer, chemotherapy, and radiation therapy can make it difficult to be physically active, modifying medication needs. These realities can make it especially challenging to manage blood glucose in the weeks during which a patient is receiving chemotherapy and/or radiation therapy.
There are no specific guidelines promulgated by the American Diabetes Association relating specifically to glycemic control during cancer therapy.4 Therefore, the approach to glycemic control during this period is similar to management during any period where disease or treatment may destabilize glycemic control. A cornerstone of management during such periods involves closer home glucose monitoring than usual. The diabetes care provider should make a management plan for this time period, including:
- Specific instructions for frequency of monitoring and the appropriate response to above and below threshold glucose values;
- Sick day management for days when oral intake is very low, including which medications to continue, which to decrease, and which to omit;
- Glucose values which require immediate outreach to the physician or emergency care should the physician be unreachable; and
- Office visit or telehealth visit frequency to communicate progress.
A common occurrence during cancer chemotherapy or radiation therapy is that the patient is too tired to continue to see the primary care provider or other physician or nurse practitioner who usually manages the diabetes. Alternatively, some patients assume that their oncologist will manage their diabetes. Since diabetes out of control is a common reason why patients with diabetes who are undergoing chemotherapy or radiation therapy are unable to complete full courses of chemotherapy,1 it is important to stress to the patient that they need to continue ongoing care for their glycemic control during cancer chemotherapy, and that the oncology care team cannot provide such management.
References
- Goldman, J.W., M.A. Mendenhall, and S.R. Rettinger, Hyperglycemia Associated With Targeted Oncologic Treatment: Mechanisms and Management. Oncologist, 2016. 21(11): p. 1326-1336.
- Nolden, A.A., et al., Chemosensory Changes from Cancer Treatment and Their Effects on Patients’ Food Behavior: A Scoping Review. Nutrients, 2019. 11(10): p. 2285.
- Ravasco, P., Nutrition in Cancer Patients. J Clin Med, 2019. 8(8).
- Association, A.D., Introduction: Standards of Medical Care in Diabetes—2022. Diabetes Care, 2021. 45(Supplement_1): p. S1-S2