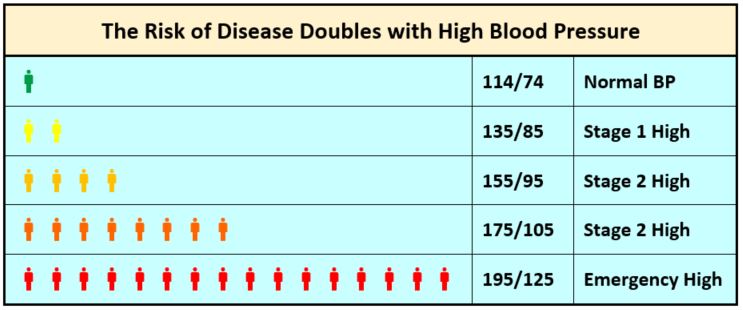
The risk for heart attack, stroke and other high blood pressure complications begins to increase around 115/75 mm Hg.1-5 The risk doubles for each 20 mm Hg increase in the systolic pressure and each 10 mm Hg increase in the diastolic pressure.1-5
Evidence shows that lowering blood pressure (BP) decreases the risk of adverse cardiovascular outcomes such as heart disease, stroke, and death.1,6-9 It may also slow the progression of kidney damage in people with chronic kidney disease (CKD).10 Further, meta-analyses as well as national and international guidelines suggest that lowering BP decreases risk of these outcomes regardless of which agent is used.1,6-9,11
Angiotensin receptor blockers (ARBs) as antihypertensive therapy have been shown to reduce the risk of cardiovascular disease (CVD), including myocardial infarction (MI),11 heart failure,11-17 and stroke.11,18 Additionally, ARBs may slow the progression of chronic kidney disease (CKD) to end-stage renal disease (ESRD).19-25
Cardiovascular Disease Risk Reduction
Bangalore et al. performed a meta-analysis of 106 randomized trials of 254,301 patients without heart failure (including placebo-controlled, active-controlled, and head-to-head trials) that compared two first-line antihypertensive monotherapies, angiotensin-converting enzyme (ACE) inhibitors and ARBs.11 The analysis found that both ARBs and ACE inhibitors significantly reduce the outcomes of all-cause mortality, cardiovascular death, and MI compared to placebo. ARBs compared to placebo significantly reduced the risk of heart failure (relative risk [RR] 0.89, 95% confidence interval [CI] [0.82 – 0.96]), stroke (RR 0.91, 95% CI [0.85 – 0.97]), end-stage renal disease (ESRD) (RR 0.81, 95% CI [0.70 – 0.94), and new-onset diabetes (RR 0.89, 95% CI [0.84 – 0.95]). In the initial analysis, ACE inhibitors but not ARBs, showed a significant reduction in all-cause mortality, cardiovascular death, and MI. The authors performed a meta-regression analysis that restricted the trials to those performed after 2000 to explore this discrepancy in findings. They found that the lower the placebo event rate, the higher the chance that the ACE inhibitor or ARB vs placebo would have no benefit for MI (p=0.001), cardiovascular death (p<0.001), and all-cause mortality (p<0.001). The meta-regression analysis concluded that ARBs actually had similarly significant reductions of risk as the ACE inhibitors did in the original analysis. In the original analysis, ACE inhibitors had a significant reduction in the risk of MI (RR 0.83, 95% CI [0.78 – 0.90]), cardiovascular death (RR 0.85, 95% CI [0.79 – 0.92]), and all-cause mortality (RR 0.91, 95% CI [0.86 – 0.96]).
A Cochrane systematic review26 of nine studies (n=11,007 hypertensives) comparing the outcomes of all-cause mortality and total CVD events (CVD-related death, stroke, MI, and heart disease) of ACE inhibitors versus ARBs as therapy for primary hypertension found no significant difference in these outcomes between the two agents.
A 2015 meta-analysis which compared different long-term antihypertensive therapies showed a significant reduction in the summary risk ratio of stroke for ARBs (RR 0.83 (95% CI [0.59 – 1.18], p=0.30) compared to beta blockers (RR 1.42, 95% CI [1.26 – 1.61], p<0.01), ACE inhibitors (RR 1.01, 95% CI [0.81 – 1.27], p=0.92), combined ACE inhibitor/ARB therapy (RR 0.94, 95% CI [0.78 – 1.13], p=0.51), thiazide or thiazide-like diuretics (RR 0.90, 95% CI [0.75 – 1.08], p=0.25), and calcium channel blockers (RR 0.83, 95% CI [0.79 – 0.89], p<0.01).18 The ARB cohort had 7,278 patients with a mean follow-up of 42.9 ± 15 months.
In addition to their role in the management of hypertension, heart failure management guidelines recommend the inhibition of angiotensin by an ACE inhibitor or ARB as a key component of the treatment plan for people with hypertension and heart failure with reduced ejection fraction (HFrEF).27-29 Studies have shown ARBs may reduce heart failure hospitalizations and death in people with HFrEF and have less incidence of cough or angioedema side effects than ACE inhibitor.12-17
Kidney Disease Risk Reduction
Studies have shown the progression of kidney disease may be slowed by angiotensin receptor blockers (ARBs) by reducing blood pressure, reducing proteinuria, improving renal blood flow, and improving interglomerular pressure due to the vasodilatory effects of ARBs.19-24
A 2016 systematic review and meta-analysis reviewed 119 randomized controlled trials of patients (n=64,768) with CKD treated with ARBs or ACE inhibitors.25 The analysis found that ARBs lowered the risk of kidney failure by 30% (odds ratio [OR] 0.70, 95% CI [0.52 – 0.89]) compared to placebo.
A 2015 network meta-analysis found ARB monotherapy significantly reduced progression to end-stage renal disease in people with diabetes compared to placebo (OR 0.77, 95% CI [0.65 – 0.92]).19 Combination therapy with ARB and ACE inhibitor was superior (OR 0.62, 95% CI [0.43 – 0.90]), but this combination has some risk of increased hyperkalemia and acute kidney injury.
A 2008 meta-analysis of 49 studies with 6,181 patients with or without diabetes and with microalbuminuria or proteinuria examined the effect of ARBs versus placebo and alternative treatments on proteinuria.24 Over one to four months, ARBs lowered proteinuria compared with placebo (ratio of means 0.57, 95% CI [0.47 – 0.68]) and over 5 to 12 months (ratio of means 0.66, CI [0.63 – 0.69]).
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360 (9349): 1903-1913.
- Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014; 383 (9932): 1899-1911.
- Reboussin DM, Allen NB, Griswold ME, et al. Systematic review for the 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017.
- Wright JT, Jr., Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373 (22): 2103-2116.
- Ahluwalia M, Bangalore S. Management of hypertension in 2017: targets and therapies. Curr Opin Cardiol 2017; 32 (4): 413-421.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. JAMA 2014; 311 (5): 507-520.
- Pignone M, Viera AJ. Blood pressure treatment targets in adults aged 60 years or older. Ann Intern Med 2017; 166 (6): 445-445.
- Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med 2017; 166 (6): 430-430.
- KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl (2011) 2013; 3 (1): i-150.
- Bangalore S, Fakheri R, Toklu B, Ogedegbe G, Weintraub H, Messerli FH. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in patients without heart failure? Insights from 254,301 patients from randomized trials. Mayo Clin Proc 2016; 91 (1): 51-60.
- Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001; 345 (23): 1667-1675.
- Pfeffer MA, McMurray JJV, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med 2003; 349 (20): 1893-1906.
- Pfeffer MA, Swedberg K, Granger CB, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet 2003; 362 (9386): 759-766.
- Konstam MA, Neaton JD, Dickstein K, et al. Effects of high-dose versus low-dose losartan on clinical outcomes in patients with heart failure (HEAAL study): a randomised, double-blind trial. Lancet; 374 (9704): 1840-1848.
- Yusuf S, Teo K, Anderson C, et al. Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomised controlled trial. Lancet 2008; 372 (9644): 1174-1183.
- Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358 (15): 1547-1559.
- Mukete BN, Cassidy M, Ferdinand KC, Le Jemtel TH. Long-term anti-hypertensive therapy and stroke prevention: a meta-analysis. Am J Cardiovasc Drugs 2015; 15 (4): 243-257.
- Palmer SC, Mavridis D, Navarese E, et al. Comparative efficacy and safety of blood pressure-lowering agents in adults with diabetes and kidney disease: a network meta-analysis. Lancet 2015; 385 (9982): 2047-2056.
- Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345 (12): 861-869.
- Woo KT, Choong HL, Wong KS, et al. Aliskiren and losartan trial in non-diabetic chronic kidney disease. J Renin Angiotensin Aldosterone Syst 2014; 15 (4): 515-522.
- Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345 (12): 851-860.
- Kobori H, Mori H, Masaki T, Nishiyama A. Angiotensin II blockade and renal protection. Curr Pharm Des 2013; 19 (17): 3033-3042.
- Kunz R, Friedrich C, Wolbers M, Mann JF. Meta-analysis: effect of monotherapy and combination therapy with inhibitors of the renin angiotensin system on proteinuria in renal disease. Ann Intern Med 2008; 148 (1): 30-48.
- Xie X, Liu Y, Perkovic V, et al. Renin-angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a Bayesian network meta-analysis of randomized clinical trials. Am J Kidney Dis 2016; 67 (5): 728-741.
- Li EC, Heran BS, Wright JM. Angiotensin converting enzyme (ACE) inhibitors versus angiotensin receptor blockers for primary hypertension. Cochrane Database Syst Rev 2014; (8): Cd009096.
- Rosendorff C, Lackland DT, Allison M, et al. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. Circulation 2015; 131 (19): e435-470.
- Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2016; 68 (13): 1476-1488.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62 (16): e147-239.

.png)
