The 2018 American Heart Association/American College of Cardiology (AHA/ACC) Guideline on the Management of Blood Cholesterol strongly recommends initiation of statin therapy for prevention and treatment of atherosclerotic heart disease (ASCVD).1 People with diagnosed ASCVD are treated with statins to prevent further cardiovascular events (secondary prevention). This includes people with acute coronary syndrome, individuals with history of myocardial infarction (MI), stable or unstable angina. It also includes those with coronary or other arterial revascularization, stroke, transient ischemic attack, or peripheral artery disease including aortic aneurysm, all of atherosclerotic origin. People who have been diagnosed with heart failure with decreased ejection fraction may also benefit from statins.
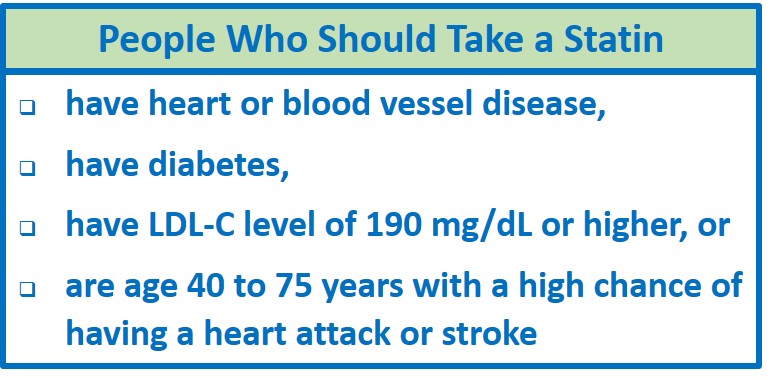
Some people who have not yet been diagnosed with ASCVD should be treated with statins to prevent a first cardiovascular event from occurring (primary prevention).1 The 2018 ACA/AHA guidelines provide levels of recommendations for the use of statins (from strong to weak), based on the degree to which the benefit of an intervention outweighs the risk, and the level of evidence that supports the recommendation.
Primary Prevention
The AHA/ACC guidelines strongly recommend that adults 40 to 75 years of age who are at intermediate-risk or higher (≥7.5%) of developing ASCVD and who have low-density lipoprotein- C (LDL-C) levels 70 – 189 mg/dl be considered for moderate or high intensity statin therapy.1 The recommendation is based on systematic reviews and meta-analyses by the Cochrane Database2 (n= 56,934) and the US Preventive Services Task Force3 (n=71,344) that found statin therapy was associated with reduced risk for ASCVD events in people at risk, but without prior history of CVD events. The level of risk for future ASCVD events should be discussed between the patient and provider to determine the intensity of statin therapy and the goals for LDL-C reduction. Ten-year risk of a significant ASCVD event can be estimated using the pooled cohort equation to categorize an individual’s risk from low (<5%) to high (≥20%). Clinician and patient together can weigh the risk, lifestyle changes that can reduce risk, and the risk-benefit ratio of initiating statin therapy. The potential for drug adverse effects, drug-drug interactions, and the patient’s preferences should be included in the decision.
Some benefit may be achieved by starting statin therapy in individuals whose ASCVD risk is borderline (5% to <7.5%).1 Again, the clinician-patient risk discussion should govern the decision.
Secondary Prevention
The guidelines strongly recommend that patients who have been diagnosed with ASCVD and are under 75 years of age be started on high-intensity statin therapy with the goal of lowering LDL-C by 50%.1 The recommendation is based on strong evidence that lowering LDL-C levels reduces ASCVD risk and that high-intensity statins are more effective in lowering that risk.4,5 Moderate-intensity statin therapy is strongly recommended if high-intensity therapy is not tolerated. Other drugs, including ezetimibe and PCSK9 inhibitors, may be considered if the individual is deemed to be at very high risk and statins alone are not effective in meeting LDL-C lowering goals. Ezetimibe and PCSK9 inhibitors added to statin therapy demonstrated additional net benefit in similar high-risk patients in three randomized controlled trials.6–8 People who are at higher risk include people who have had more than one major ASCVD event or one major event with other high-risk conditions, including age over 65, current smoking, diabetes, hypertension, chronic kidney disease, heterozygous familial hypercholesterolemia, or a history of coronary artery bypass surgery, percutaneous coronary intervention, or congestive heart failure, as well as a persistently elevated LDL-C over 100 mg/dL despite statins and ezetimibe.1
Hypercholesterolemia
The guidelines also strongly recommend that adults 20 to 75 years of age with severe hypercholesterolemia (LDL-C 190 mg/dL or higher) take maximally tolerated statins.1 Individuals with elevated levels of LDL-C have a high-risk of ASCVD.9 In a placebo-controlled primary prevention study of pravastatin in 6,595 men with LDL-C levels 192 ± 17 mg/dL, Shepard et al. showed a significantly reduced incidence of MI or coronary death in men taking the statin (relative reduction in risk with pravastatin 31%, 95% confidence interval [17% – 43%], p<0.001).10 A post-hoc analysis of 2,560 men without evidence of vascular disease from the same cohort assessed incidence of ASCVD events and mortality over 20 years of follow-up and found that pravastatin reduced the risk of coronary heart disease by 27% (p=0.002).11
If necessary to reach the goal of 50% reduction of LDL-C in people with hypercholesterolemia, ezetimibe, bile acid sequestrants, or PCSK9 inhibitors can also be considered in some circumstances, but the strength of the recommendation and the quality of the evidence for these added medications is less strong.1
Patients with Diabetes
Moderate intensity statin therapy is strongly recommended for patients with diabetes mellitus who are 40 to 75 years of age, regardless of their LDL-C levels or their 10-year risk of ASCVD.1 Generally, diabetics in this age range are at intermediate or high-risk of ASCVD12 and statins have been shown to reduce this risk.13,14 Although the evidence is less strong, as diabetics age, they may accrue additional risk factors and it is reasonable to consider a 10-year risk of ASCVD events using a pooled cohort equation to determine the intensity of statin therapy or the addition of other medications.1,12 The pooled cohort equation is a risk calculator that was developed and validated among black and Caucasian men and women without clinical ASCVD to estimate future risk of cardiovascular events.15 In adult diabetics who are younger than 40 years of age, it is reasonable to consider statin therapy depending on duration of diabetes, kidney function, and other clinical factors that enhance the risk of ASCVD.1
Other Populations Who May Benefit from Statins
The 2018 AHA/ACC Guidelines for Management of Blood Cholesterol recommends statins be considered for young people (age 0 – 19) diagnosed with familial hypercholesterolemia and adults (aged 20 – 39) with a family history of premature ASCVD and LDL-C levels over 160 mg/dL.1 Other risk-enhancing conditions that favor the use of statins in people whose risk is ≥7.5% are chronic inflammatory disorders, HIV, metabolic syndrome, chronic renal disease, premature menopause, South Asian ancestry, and elevated biomarkers including high-sensitivity C-reactive protein, triglycerides, lipoprotein (a), or apolipoprotein B levels.
References
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol. J Am Coll Cardiol 2019; 73(24).
- Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease (Review). Cochrane Database Syst Rev 2013;(1): 1-97.
- Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016; 316 (19): 2008-2024.
- Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet 2010; 376 (9753): 1670-1681.
- Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016; 388 (10059): 2532-2561.
- Cannon C, Blazing M, Giugliano R et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 2015; 372 (25): 2387-2397.
- Sabatine M, Giugliano R, Wiviott S, Al E. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med 2015; 372 (16): 1500-09.
- Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med 2018; 379 (22): 2097-2107.
- Perak AM, Ning H, de Ferranti SD, Gooding HC, Wilkins JT, Lloyd-Jones DM. Long-term risk of atherosclerotic cardiovascular disease in US adults with the familial hypercholesterolemia phenotype. Circulation 2016; 134 (1): 9-19.
- Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med 1995; 333 (20): 1301-1307.
- Vallejo-Vaz AJ, Robertson M, Catapano AL, et al. Low-density lipoprotein cholesterol lowering for the primary prevention of cardiovascular disease among men with primary elevations of low-density lipoprotein cholesterol levels of 190 mg/dL or above: analyses from the WOSCOPS (West of Scotland Coronary Prevention Study) 5-year randomized trial and 20-year observational follow-up. Circulation 2017; 136 (20): 1878-1891.
- Wong ND, Glovaci D, Wong K, et al. Global cardiovascular disease risk assessment in United States adults with diabetes. Diabetes Vasc Dis Res 2012; 9 (2): 146-152.
- Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet (London, England) 2004; 364 (9435): 685-696.
- de Vries FM, Denig P, Pouwels KB, Postma MJ, Hak E. Primary prevention of major cardiovascular and cerebrovascular events with statins in diabetic patients: a meta-analysis. Drugs 2012; 72 (18): 2365-2373.
- Yadlowsky S, Hayward RA, Sussman JB, McClelland RL, Min Y-I, Basu S. Clinical implications of revised pooled cohort equations for estimating atherosclerotic cardiovascular disease risk. Ann Intern Med 2018; 169 (1): 20-29.