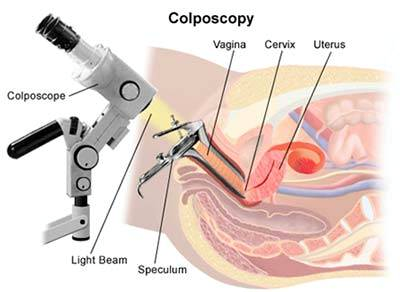
A colposcopy is a procedure that is performed when the screening pap smear is abnormal. 1 During a colposcopy an instrument called a colposcope is used to visualize both cervix and vagina. 2 Visual characterization of the magnified genital tract allows for guided biopsy of abnormal areas and histologic diagnosis. The purpose of colposcopy is to distinguish women at high risk for cervical cancer who need treatment from women at low risk who may undergo surveillance. 3
After magnification and illumination of the entire cervix and upper vagina, 3% to 5% acetic acid (table vinegar) or Lugol’s iodine solution can be applied to the genital tract to assess for abnormalities. Application of acetic acid leads to dehydration of cells and coagulation of proteins which visually turns epithelial cells white. This occurs more distinctly in abnormal epithelial cells due to their high protein density and highlights these abnormal lesions for potential biopsy.4 Lugol’s iodine works in the opposite fashion, staining glycogen contained in normal cells a dark color and leaving abnormal cells that lack glycogen unstained.5 Thus, when using Lugol iodine, unstained areas are indicative of abnormal cells concerning precancerous lesions. Based on these characteristics, a biopsy can be taken of the most abnormal appearing lesion. Notably, a study by Wentzensen et al. found that multiple, targeted biopsies increased the sensitivity of colposcopy from 60.6% to 95.6% compared to taking a single, targeted biopsy.6 Therefore, the American Society for Colposcopy and Cervical Pathology recommends a risk-based approach whereby multiple biopsies may be taken if a patient has risk factors such as HPV positivity, higher-grade referral cytology, or a more severe colposcopic impression.3 If biopsy results demonstrate low-grade dysplasia, then surveillance pap smears in 6-12 months are generally sufficient. If biopsy results demonstrate high-grade dysplasia, then ablative procedures (cryotherapy) or excisional procedures (Loop Electrosurgical Excision Procedure or Cervical Conization) are performed. Rarely, cancer is diagnosed, and patients are referred to cancer specialists for further care.
In the United States, about 1.2 million women are evaluated by colposcopy each year.7 Together with Pap smear screening tests and treatment of precancerous lesions, colposcopy is essential for the prevention and treatment of cervical cancer.2 Colposcopy not only identifies cervical precancer and early invasive cancer but also prevents overtreatment of benign lesions. Additionally, procedural risks such as bleeding, infection, and long-term morbidity are low.2 While some psychological harms such as anxiety and fear of pain have been noted in the literature, these harms can be minimized with certain interventions.8 Playing music during the procedure as well as the use of video colposcopy can significantly reduce anxiety and pain experienced during the procedure.9,10
References
- Massad LS, Einstein MH, Huh WK, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet Gynecol. 2013;121(4):829-846. doi:10.1097/AOG.0b013e3182883a34
- Khan MJ, Werner CL, Darragh TM, et al. ASCCP colposcopy standards: role of colposcopy, benefits, potential harms, and terminology for colposcopic practice. J Low Genit Tract Dis. 2017;21(4):223-229. doi:10.1097/LGT.0000000000000338
- Wentzensen N, Massad LS, Mayeaux EJ, et al. Evidence-based consensus recommendations for colposcopy practice for cervical cancer prevention in the United States. J Low Genit Tract Dis. 2017;21(4):216-222. doi:10.1097/LGT.0000000000000322
- Sankaranarayanan R, Wesley R, Somanathan T, et al. Visual inspection of the uterine cervix after the application of acetic acid in the detection of cervical carcinoma and its precursors. Cancer. November 1998.
- El-Shalakany AH, Saeed MM, Abdel-Aal MR, et al. Direct visual inspection of the cervix with Lugol iodine for the detection of premalignant lesions. J Low Genit Tract Dis. 2008;12(3):193-198. doi:10.1097/LGT.0b013e31815f527c
- Wentzensen N, Walker JL, Gold MA, et al. Multiple biopsies and detection of cervical cancer precursors at colposcopy. J Clin Oncol. 2015;33(1):83-89. doi:10.1200/JCO.2014.55.9948
- Saraiya M, McCaig LF, Ekwueme DU. Ambulatory care visits for Pap tests, abnormal Pap test results, and cervical cancer procedures in the United States. Am J Manag Care. 2010;16(6):e137-44.
- Bekkers RLM, van der Donck M, Klaver FM, van Minnen A, Massuger LFAG. Variables influencing anxiety of patients with abnormal cervical smears referred for colposcopy. J Psychosom Obstet Gynaecol. 2002;23(4):257-261. doi:10.3109/01674820209074680
- Chan YM, Lee PWH, Ng TY, Ngan HYS, Wong LC. The use of music to reduce anxiety for patients undergoing colposcopy: a randomized trial. Gynecol Oncol. 2003;91(1):213-217. doi:10.1016/s0090-8258(03)00412-8
- Walsh JC, Curtis R, Mylotte M. Anxiety levels in women attending a colposcopy clinic: a randomised trial of an educational intervention using video colposcopy. Patient Educ Couns. 2004;55(2):247-251. doi:10.1016/j.pec.2003.09.012