Evidence shows that lowering blood pressure (BP) decreases the risk of adverse cardiovascular outcomes such as heart disease, stroke, and death.1-5 It may also slow the progression of kidney damage in people with chronic kidney disease (CKD).6 Further, meta-analyses as well as national and international guidelines suggest that lowering BP decreases risk of these outcomes regardless of which agent is used.1-5,7
Angiotensin-converting enzyme (ACE) inhibitors are a first-line treatment for all stages of hypertension as a monotherapy or in combination with one or more other antihypertensive agents.1-5,8 Studies have found no significant efficacy differences between the individual ACE inhibitors.8,9
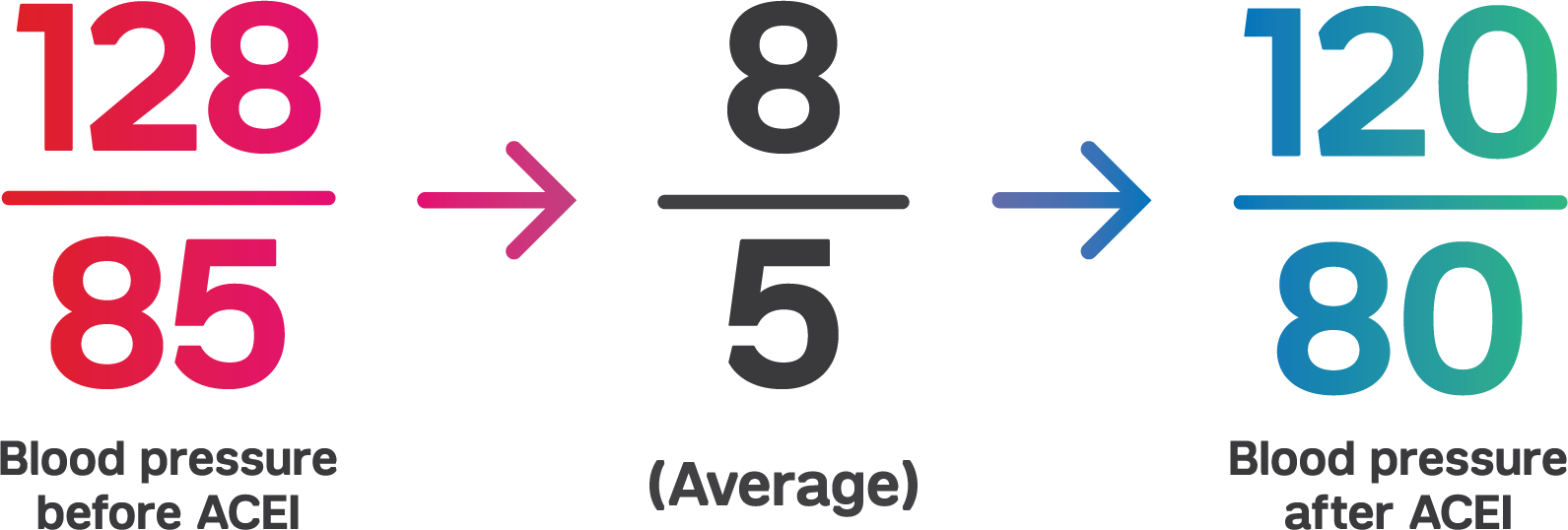
Monotherapy trials show the BP lowering efficacy of ACE inhibitors.10-15 A 2008 Cochrane Review meta-analysis found 92 randomized controlled trials (RCTs) that studied the dose-related trough BP lowering efficacy of 14 ACEIs in 12,954 participants.8 The baseline BP was 157/101 mm Hg across the trials. ACE inhibitors lowered BP measured one to 12 hours after the dose by about 11/6 mm Hg. The best estimate or trough BP lowering effect for ACEIs based on the largest trials was -8 mm Hg for systolic blood pressure and -5 mm Hg for diastolic blood pressure. The analysis also found that a dose of 50% of the maximum (max) daily dose had a BP lowering effect that was 90% of max and that ACE inhibitor doses above the max dose did not lower BP significantly any more than the max dose.
A 2015 meta-analysis of five major antihypertensive drug classes found 12 RCTs and 13 randomized comparisons (35,707 patients) in which an ACE inhibitor was the active treatment drug.16 The review found that an systolic BP/diastolic BP difference of about -4/-2 mm Hg between ACE inhibitor therapy versus placebo was associated with significant reductions in the relative risk of all outcomes, except cardiovascular and all-cause mortalities. The analysis found that stroke was reduced by –20% (–7 to –31%), heart failure by –21% (–7 to –34%), coronary heart disease (CHD) by –13% (–3 to –21%) and major cardiovascular events (composite of stroke, CHD and heart failure) by –17% (–8 to 25%). Cardiovascular mortality (11% reduction) and all-cause mortality (8% reduction) did not achieve statistical significance.
A 2011 Cochrane Review meta-analysis found four RCTs (three comparing ACE inhibitors to placebo and one comparing ACE inhibitors with angiotensin receptor blockers [ARBs]) with a total 2,177 participants that reported the effect of ACE inhibitors on people with early (stage 1 to 3) CKD who do not have diabetes mellitus.17 The review concluded that there is insufficient evidence showing the effectiveness of ACE inhibitors in preventing all-cause mortality or cardiovascular events in people with CKD who do not have diabetes.
However, the 2012 KDIGO clinical practice guideline recommends an ACE inhibitor or ARB be used in diabetic adults with CKD and urine albumin excretion 30 to 300 mg/24 hours.6 The guideline also recommends that an ARB or ACE inhibitor be used in both diabetic and non-diabetic adults with CKD and urine albumin excretion >300 mg/24 hours.
References
- Ahluwalia M, Bangalore S. Management of hypertension in 2017: Targets and therapies. Curr Opin Cardiol 2017; 32 (4): 413-421.
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. JAMA 2014; 311 (5): 507-520.
- Pignone M, Viera AJ. Blood pressure treatment targets in adults aged 60 years or older. Ann Intern Med 2017; 166 (6): 445-445.
- Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: A clinical practice guideline from the American college of physicians and the American Academy of Family Physicians. Ann Intern Med 2017; 166 (6): 430-430.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017.
- KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl (2011) 2013; 3 (1): i-150.
- Bangalore S, Fakheri R, Toklu B, Ogedegbe G, Weintraub H, Messerli FH. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in patients without heart failure? Insights from 254,301 patients from randomized trials. Mayo Clin Proc 2016; 91 (1): 51-60.
- Heran BS, Wong MM, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database Syst Rev 2008; (4): Cd003823.
- Powers BJ, Coeytaux RR, Dolor RJ, et al. Updated report on comparative effectiveness of ACE inhibitors, ARBs, and direct renin inhibitors for patients with essential hypertension: Much more data, little new information. J Gen Intern Med 2012; 27 (6): 716-729.
- Guitard C, Lohmann FW, Alfiero R, Ruina M, Alvisi V. Comparison of efficacy of spirapril and enalapril in control of mild-to-moderate hypertension. Cardiovasc Drugs Ther 1997; 11 (3): 449-457.
- Persson B, Stimpel M. Evaluation of the antihypertensive efficacy and tolerability of moexipril, a new ACE inhibitor, compared to hydrochlorothiazide in elderly patients. Eur J Clin Pharmacol 1996; 50 (4): 259-264.
- Gasowski J, Wilkins A, Drzewoski J, et al. Short-term antihypertensive efficacy of perindopril according to clinical profile of 3,188 patients: A meta-analysis. Cardiol J 2010; 17 (3): 259-266.
- Gradman AH, Arcuri KE, Goldberg AI, et al. A randomized, placebo-controlled, double-blind, parallel study of various doses of losartan potassium compared with enalapril maleate in patients with essential hypertension. Hypertension 1995; 25 (6): 1345-1350.
- Ionescu DD. Antihypertensive efficacy of perindopril 5-10 mg/day in primary health care: An open-label, prospective, observational study. Clin Drug Investig 2009; 29 (12): 767-776.
- Sanders GD, Coeytaux R, Dolor RJ, et al. Angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor antagonists (ARBs), and direct renin inhibitors for treating essential hypertension: An update. In: AHRQ comparative effectiveness reviews. Rockville (MD): Agency for Healthcare Research and Quality (US); 2011.
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs--overview and meta-analyses. J Hypertens 2015; 33 (2): 195-211.
- Sharma P, Blackburn RC, Parke CL, McCullough K, Marks A, Black C. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers for adults with early (stage 1 to 3) non-diabetic chronic kidney disease. Cochrane Database Syst Rev 2011; (10): Cd007751.

.png)
