Scleroderma or systemic sclerosis (SSc) is a rare systemic autoimmune disease that is characterized by vasculopathy, immune dysregulation, and fibroblast dysfunction, which can result in fibrosis in various organ systems.1 SSc is broadly categorized into two main subsets: diffuse cutaneous SSc and limited cutaneous SSc. Diffuse cutaneous SSc is characterized by extensive fibrotic disease, with skin thickening proximal to elbows, knees, and neck, as well as a high prevalence of interstitial lung disease (ILD). Limited cutaneous SSc manifests largely as a vascular disease, resulting in Raynaud phenomenon, pulmonary arterial hypertension, and skin sclerosis confined to the distal extremities.
Lung fibrosis is common among those with SSc, although exact prevalence is difficult to determine due to the rarity of the disease and regional differences in diagnostic criteria for both SSc and ILD. A population-based study in Norway taking place from 2000-2012 found that of the 815 residents with diagnosed SSc, 50% had ILD and 46% had declining pulmonary function consistent with developing ILD.2
Disease Progression and Prognosis
Organ involvement including ILD can be an early complication of SSc. A 2016 study using the European Alliance of Associations for Rheumatology Scleroderma Trial Research (EUSTAR) database (n=695) examined the time to onset of organ involvement in relation to the development of Raynaud’s phenomenon.6 FVC<50% was diagnosed in 2% of patients within the first year and in 12% during the 10-year follow-up. About 33% had DLCO<50% within three years, which progressively increased to 54% of patients over the 10-year follow-up.
A 2022 study of 89 patients with SSc-ILD explored the effect of their condition on health-related quality of life (HRQOL) using the King’s Brief Interstitial Lung Disease (KBILD, scores from 0-100, where higher scores indicate better HRQOL) HRQOL assessment questionnaire.3 The average score was 58.4, with only 9.4% of patients scoring ≥75. When broken out into the three parts of the KBILD questionnaire, average scores were 63.8 for psychology, 48.5 for breathlessness and activities, and 75.2 for chest symptoms. When ranking symptoms on a five-point scale, patients reported that fatigue was their most severe symptom with a mean score of 4.4.
SSc-ILD has a variable course; some patients have stable lung involvement whereas others have highly progressive lung involvement. A 2021 study using the European Alliance of Associations for Rheumatology Scleroderma Trial Research (EUSTAR) database showed that among patients with SSc-ILD (n=826), 33% of patients had stable lung function during 5 years of follow-up, 58% had a pattern of slow lung function decline with more periods of stability or improvement than decline, and 8% had a rapid continuous decline.4 There was no significant differences in mortality between patients with significant ILD progression (12%), moderate progression (15%), or stable ILD (9%).
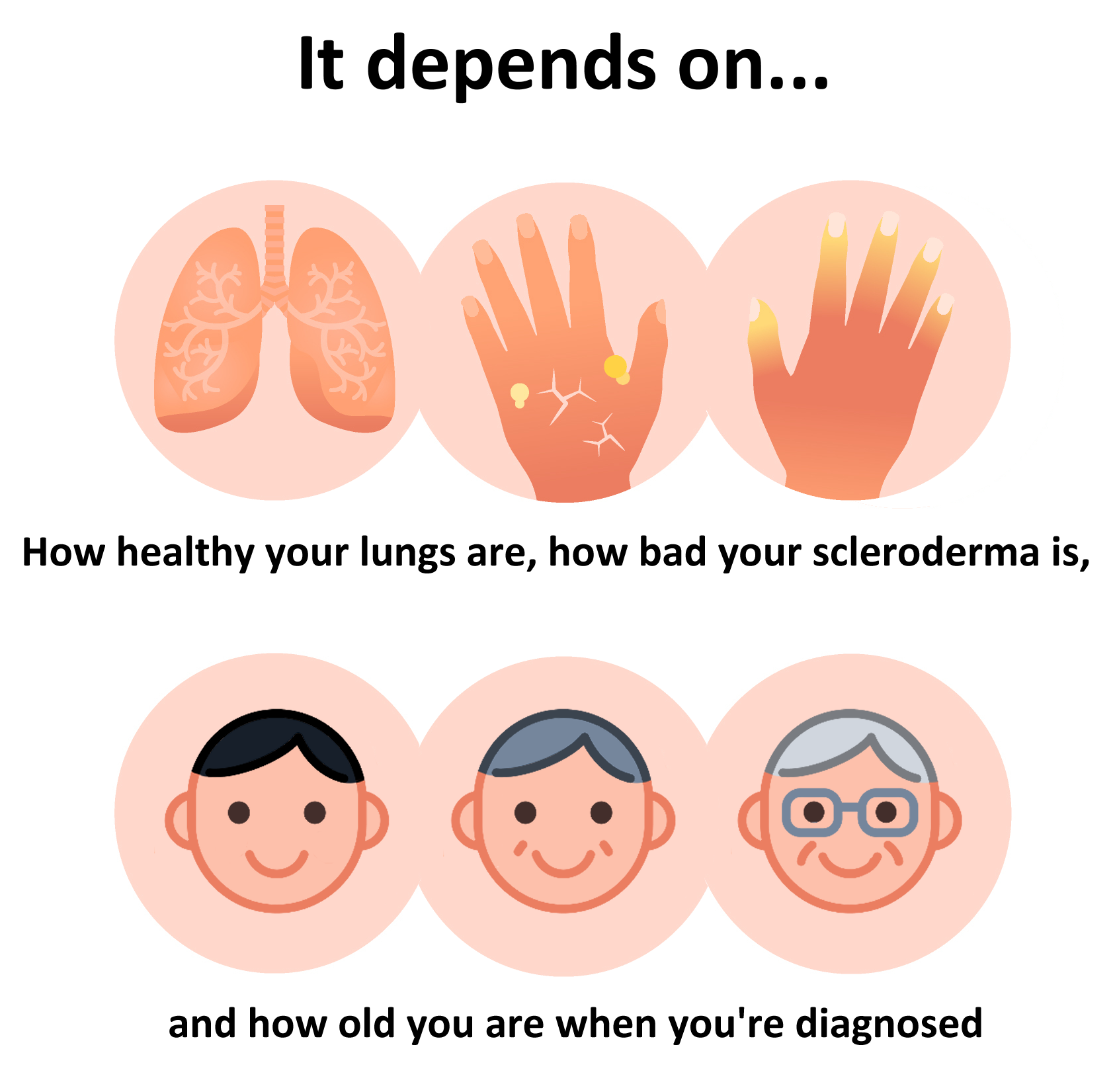
Those diagnosed with SSc later in life are more likely to have multi-organ impacts, leading to a faster disease course.5 A 2020 study of 3,281 patients in the German Network for Systemic Scleroderma compared progression among three age-at-diagnosis groups: <40 years, 40-60 years, and >60 years. Those diagnosed over the age of 60 had significantly more organ manifestation at baseline than those 40-60 years old and <40 years old, including pulmonary hypertension (19.2%, 11.8%, and 7.5%, respectively), lung fibrosis (40.7%, 35.9%, 37.5%), and heart changes (14.8%, 11.9%, 10.5%). After ten years of follow-up, fewer patients with a late disease onset (>60 years) compared to those with early onset (<40 years) were free of organ manifestation, including pulmonary hypertension (61.8% vs 90.5%), lung fibrosis (47.8% vs 56.7%), and heart involvement (62.6% vs 81.5%). The authors recommended more frequent follow-up visits for patients who are older due to risk factors of multi-organ involvement and consequent accelerated disease course.
Mortality
Predictors of disease progression and survival include forced vital capacity (FVC), diffusing capacity of carbon monoxide (DLCO), presence of anti-topoisomerase I antibodies (ATA)(also known as anti Scl-70 antibodies), extent of fibrosis, and age at diagnosis.
A cohort study of 162 patients with SSc-ILD sought to determine the predictive value of short-term pulmonary function tests (PFTs) on 15-year survival.6 There was 52% mortality during a median follow-up of 13 years, and PFTs including FVC, DLCO, carbon monoxide transfer coefficient (KCO), and the ratio of FVC:DLCO were found to be good prognostic indicators, with worse results on PFTs linked to higher rates of mortality. Among the whole cohort, survival was 30% among those with ≥10% FVC decline compared to 50% survival for those with <10% FVC (Hazard Ratio [HR] 1.84, p=0.01). When broken into subgroups based on extensive or limited lung fibrosis, those with extensive lung fibrosis and ≥10% FVC decline had <10% survival compared to 43% for <10% FVC (HR 2.31, p=0.02). Survival was relatively similar between those with limited lung fibrosis regardless of FVC at around 50% (HR 1.10, p=0.81).
In a study of 171 patients with SSc-ILD, annual changes to FVC and DLCO were found to be a significant predictor survival.7 Among those who died within <4 years, mean percent predicted FVC (ppFVC) decline was 4.10% and percent predicted DLCO (ppDLCO) decline was 5.28% compared to 2.14% ppFVC and 3.13% ppDLCO among those who survived for 4-8 years and 0.94% FVC and 1.32% DLCO among those who survived >8 years. While annual DLCO change was found to be a good predictor of DLCO change for the next 12 months, FVC was not found to be predictive of short-term future change in FVC.
Lung function decline was observed in a longitudinal study (n=184) that took place from 2011-2019.8 Overall mortality was 16.3%, with 21.6% caused by progressive ILD and 27.5% caused by pulmonary hypertension. ppFVC decline was indicative of survival, with 8.28% decline among those who died in >2 years, 3.89% for those who died withing 2-8 years, and 0.13% for those who survived. Presence of ATA was associated with ppFVC decline and ILD extent >20% was associated with ppDLCO decline.
A 2021 observational study identified risk factors associated with SSc-ILD by reviewing medical records of 380 patients with SSc, including 227 patients diagnosed with SSc-ILD based on chest high-resolution computed tomography (HRCT).9 Of the 72 patients who died during a mean follow-up of 9.6 years, 79.2% had ILD. Of those 57 patients with ILD who died, 61.5% died within the first four years of diagnosis. ILD was the leading cause of mortality for the whole cohort (33.3%) and pulmonary involvement, namely pulmonary hypertension, was the leading cause of mortality among those with ILD (52.6%). Survival was significantly worse among patients with SSc-ILD than those without (85.5% vs 91.5% at five years, 74.9% vs 91.5% at ten years, and 67.8% vs 85.8% at 15 years). Survival was significantly lower for patients with an FVC<70% at baseline compared to FVC≥70% (61% vs 82% survival at 15 years, p=0.003). The characteristics significantly associated with SSc-ILD mortality included male sex (p=0.003), disease duration <4 years (p<0.001), FVC<70% at baseline (p=0.003), and pulmonary systolic arterial pressure (PSAP) ≥40 mm Hg on echocardiography (p<0.011).
A 2005 meta-analysis of mortality rates and cause among SSc patients (n=3,111) found that lung involvement was a significant predictor of mortality, with 31.7% mortality among those with lung involvement (Hazard Ratio [HR] 1.6, p<0.001).10
Pulmonary features are commonly cited as a leading cause of death for SSc-related mortality. A study examining the cause of death in patients with SSc between 1972-1997 (n=1,109) found that 60% of scleroderma-related deaths are from either pulmonary fibrosis or pulmonary hypertension.11 Another study looking at deaths of patients with SSc from 2004-2008 (n=234) found that 33% died of pulmonary causes, including pulmonary fibrosis (19%) and isolated pulmonary hypertension (14%).12
Treatment
American Thoracic Society clinical practice guidelines recommend the use of certain immunosuppressants for the treatment of systemic sclerosis-associated interstitial lung disease (SSc-ILD).13 They strongly recommend the use of mycophenolate mofetil (MMF) and conditionally recommend cyclophosphamide (CYC), rituximab, tocilizumab, nintedanib, and nintedanib in combination with mycophenolate. They advise that there is insufficient evidence to recommend the use of pirfenidone and pirfenidone in combination with mycophenolate.
Smoking
In a 2018 study of 3,319 patients with various smoking statuses (66% never smokers, 23% ex-smokers, and 11% current smokers), smoking history and status was not indicative of mortality or progression of SSc-ILD.14 There were also no associations between smoking history and skin involvement (for limited SSc, 64% among never smokers, 62% for past smokers, and 58% for current smokers; for diffuse SSc, 29% for never smokers, 30% for past smokers, and 27% for current smokers). While there were no SSc-ILD-specific changes in progression, current smokers had a lower baseline forced expiratory volume in 1 second (FEV1) to FVC ratio (92.8 vs 97.5, p<0.001) and single-breath DLCO (67.1 vs 69.8, p<0.001). Smokers also had lower ATA when compared to never smokers and ex-smokers (31, 45 and 40, respectively).
A 2007 study (n=203) found that smokers, while not more likely to have worse disease progression, were more likely to have an obstructive lung pattern, both among current smokers (29% vs 12%, p=0.008) and those who had a history of smoking (21% vs 7%, p=0.03).15
References
- Varga J. Systemic Sclerosis (Scleroderma) and Related Disorders. In: Jameson J, Fauci A, Kasper D, Hauser S, Longo D, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 20 ed. McGraw-Hill Education; 2018.
- Hoffmann-Vold AM, Fretheim H, Halse AK, et al. Tracking Impact of Interstitial Lung Disease in Systemic Sclerosis in a Complete Nationwide Cohort. Am J Respir Crit Care Med. Nov 15 2019;200(10):1258-1266. doi:10.1164/rccm.201903-0486OC
- Allanore Y, Constans J, Godard D, et al. Quality of life in SSc-ILD patients: Understanding the impact of the ILD and the needs of the SSc-ILD patients and their need for caregivers in France. J Scleroderma Relat Disord. Feb 2022;7(1):49-56. doi:10.1177/23971983211013979
- Hoffmann-Vold AM, Allanore Y, Alves M, et al. Progressive interstitial lung disease in patients with systemic sclerosis-associated interstitial lung disease in the EUSTAR database. Ann Rheum Dis. Feb 2021;80(2):219-227. doi:10.1136/annrheumdis-2020-217455
- Moinzadeh P, Kuhr K, Siegert E, et al. Older age onset of systemic sclerosis – accelerated disease progression in all disease subsets. Rheumatology. 2020;59(11):3380-3389. doi:10.1093/rheumatology/keaa127
- Goh NS, Hoyles RK, Denton CP, et al. Short‐Term Pulmonary Function Trends Are Predictive of Mortality in Interstitial Lung Disease Associated With Systemic Sclerosis. Arthritis & Rheumatology. 2017;69(8):1670-1678. doi:10.1002/art.40130
- Guler SA, Winstone TA, Murphy D, et al. Does Systemic Sclerosis–associated Interstitial Lung Disease Burn Out? Specific Phenotypes of Disease Progression. Annals of the American Thoracic Society. 2018;15(12):1427-1433. doi:10.1513/AnnalsATS.201806-362OC
- Ramahi A, Lescoat A, Roofeh D, et al. Risk factors for lung function decline in systemic sclerosis-associated interstitial lung disease in a large single-centre cohort. Rheumatology. 2023;62(7):2501-2509. doi:10.1093/rheumatology/keac639
- de Oliveira Martins LV, Oliveira SM, Silvatti J, de Amorim FG, Agapito Tito CV, Kayser C. Mortality in Systemic Sclerosis–Associated Interstitial Lung Disease in Brazil. JCR: Journal of Clinical Rheumatology. 2022;28(2):e532-e538. doi:10.1097/rhu.0000000000001792
- Ioannidis JP, Vlachoyiannopoulos PG, Haidich AB, et al. Mortality in systemic sclerosis: an international meta-analysis of individual patient data. Am J Med. Jan 2005;118(1):2-10. doi:10.1016/j.amjmed.2004.04.031
- Steen VD, Medsger TA. Changes in causes of death in systemic sclerosis, 1972-2002. Ann Rheum Dis. Jul 2007;66(7):940-4. doi:10.1136/ard.2006.066068
- Tyndall AJ, Bannert B, Vonk M, et al. Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis. Oct 2010;69(10):1809-15. doi:10.1136/ard.2009.114264
- Raghu G, Montesi SB, Silver RM, et al. Treatment of Systemic Sclerosis-associated Interstitial Lung Disease: Evidence-based Recommendations. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. Sep 29 2023;doi:10.1164/rccm.202306-1113ST
- Jaeger VK, Valentini G, Hachulla E, et al. Brief Report: Smoking in Systemic Sclerosis: A Longitudinal European Scleroderma Trials and Research Group Study. Arthritis & Rheumatology. 2018;70(11):1829-1834. doi:10.1002/art.40557
- McNearney TA, Reveille JD, Fischbach M, et al. Pulmonary involvement in systemic sclerosis: associations with genetic, serologic, sociodemographic, and behavioral factors. Arthritis Rheum. Mar 15 2007;57(2):318-26. doi:10.1002/art.22532