[NOTE: This article has been posted prior to peer review for use in an active research program. This content will be updated with a peer reviewed version as soon as it is available.]
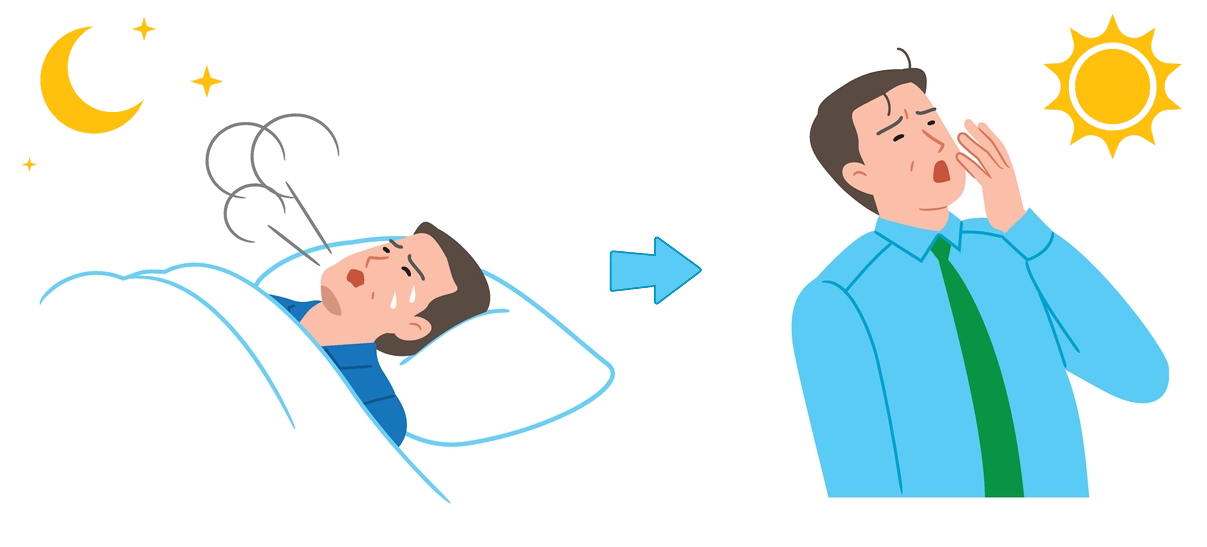
Chronic obstructive pulmonary disease (COPD) is associated with high rates of sleep disturbance. In large patient surveys, over 70% of individuals with COPD report difficulty falling or staying asleep, waking during the night, or waking up feeling unrefreshed.1 These symptoms are more common in COPD patients than in healthy individuals, with a control study finding that 68% of people with stable COPD screened positive for at least one sleep disorder, compared to 16% of matched controls.2. Poor sleep in COPD is associated with worsened symptom control, increased hospitalizations,3 and greater cardiovascular risk.4,5
The exact mechanisms that cause poor sleep quality in patients living with COPD are not fully understood.6 Patients with COPD more frequently report decreased time in deep and REM sleep.7,8 Shortness of breath, particularly when lying flat, makes sleep initiation and maintenance difficult. Nocturnal coughing, wheeze and mucus production, which may be more pronounced due to airway inflammation, can cause frequent awakenings.9,10 Hypoventilation in COPD leads to hypercapnia, which can cause arousal during sleep.11 Predisposing factors, such as aging and smoking, promote the development of obstructive apnea.6
COPD is linked to abnormalities in both respiratory mechanics and gas exchange. During sleep, the wakefulness drive to breathe is lost, leading to reduced ability to compensate for respiratory load, higher airway resistance, and hypoventilation, even in healthy individuals.12 In people with COPD, these effects are amplified due to intrathoracic airway narrowing and lung hyperinflation, which further increase airflow resistance and elastic loading.13 As a result, those with impaired respiratory mechanics may struggle to adapt to these changes and experience worsening respiratory function during sleep, causing sleep fragmentation and insomnia.
Importantly, while medications like corticosteroids or beta-agonists may sometimes cause sleep disturbance, these medications are critical to disease control.14,15 Patients should not stop or alter their treatment without consulting their healthcare provider. Rather, attention to nighttime symptoms, good sleep hygiene, and regular discussion of sleep during clinical visits may offer important opportunities for improving both COPD and cardiovascular outcomes.16
In summary, sleep disturbance is highly prevalent in COPD, driven by COPD related symptoms and nocturnal hypoventilation. Poor sleep is not just a quality-of-life issue. It may accelerate disease progression and increase cardiovascular risk. Sleep assessment and support should be a routine part of COPD care.
References
- Ding B, Small M, Holmgren U. A cross-sectional survey of current treatment and symptom burden of patients with COPD consulting for routine care according to GOLD 2014 classifications. Int J Chron Obstruct Pulmon Dis. 2017;12:1527-1537. doi:10.2147/COPD.S133793
- Vaidya S, Gothi D, Patro M. Prevalence of sleep disorders in chronic obstructive pulmonary disease and utility of global sleep assessment questionnaire: An observational case-control study. Ann Thorac Med. 2020;15(4):230-237. doi:10.4103/atm.ATM_85_20
- Borel JC, Pepin JL, Pison C, et al. Long-term adherence with non-invasive ventilation improves prognosis in obese COPD patients. Respirology. Aug 2014;19(6):857-65. doi:10.1111/resp.12327
- Shorofsky M, Bourbeau J, Kimoff J, et al. Impaired Sleep Quality in COPD Is Associated With Exacerbations: The CanCOLD Cohort Study. Chest. Nov 2019;156(5):852-863. doi:10.1016/j.chest.2019.04.132
- Baugh A, Buhr RG, Quibrera P, et al. Risk of COPD exacerbation is increased by poor sleep quality and modified by social adversity. Sleep. Aug 11 2022;45(8)doi:10.1093/sleep/zsac107
- McNicholas WT, Verbraecken J, Marin JM. Sleep disorders in COPD: the forgotten dimension. Eur Respir Rev. Sep 1 2013;22(129):365-75. doi:10.1183/09059180.00003213
- McSharry DG, Ryan S, Calverley P, Edwards JC, McNicholas WT. Sleep quality in chronic obstructive pulmonary disease. Respirology. Oct 2012;17(7):1119-24. doi:10.1111/j.1440-1843.2012.02217.x
- Saaresranta T, Irjala K, Aittokallio T, Polo O. Sleep quality, daytime sleepiness and fasting insulin levels in women with chronic obstructive pulmonary disease. Respir Med. Jul 2005;99(7):856-63. doi:10.1016/j.rmed.2004.11.017
- DP S, RT J, K M. Nocturnal Cough. In: StatPearls. 2025;
- Klink M, Quan SF. Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest. Apr 1987;91(4):540-6. doi:10.1378/chest.91.4.540
- Hedemark LL, Kronenberg RS. Ventilatory and heart rate responses to hypoxia and hypercapnia during sleep in adults. J Appl Physiol Respir Environ Exerc Physiol. Aug 1982;53(2):307-12. doi:10.1152/jappl.1982.53.2.307
- Orem J. The nature of the wakefulness stimulus for breathing. Prog Clin Biol Res. 1990;345:23-30; discussion 31.
- Skatrud JB, Dempsey JA, Badr S, Begle RL. Effect of airway impedance on CO2 retention and respiratory muscle activity during NREM sleep. J Appl Physiol (1985). Oct 1988;65(4):1676-85. doi:10.1152/jappl.1988.65.4.1676
- Cole JL. Steroid-Induced Sleep Disturbance and Delirium: A Focused Review for Critically Ill Patients. Fed Pract. Jun 2020;37(6):260-267.
- Klugherz LJ, Mansukhani MP, Kolla BP. Effects of Commonly Prescribed Medications on Sleep: A Review of the Literature. Mayo Clin Proc. May 2025;100(5):856-867. doi:10.1016/j.mayocp.2025.02.005
- Association AH. Sleep. American Heart Association. Accessed August 11, 2025. https://www.heart.org/en/healthy-living/healthy-lifestyle/sleep