Multiple studies on chronic heart failure patients have shown that carvedilol is effective in reducing the risk of death and hospitalization.1-4 Because the guidelines note that carvedilol is the preferred antihypertensive for patients with heart failure with reduced ejection fraction (HFrEF), landmark studies included here were conducted on patients with chronic heart failure.
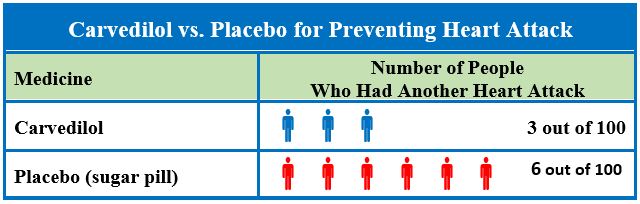
The Carvedilol Post-Infarct Survival Control in Left Ventricular Dysfunction (CAPRICORN) study measured outcomes of 1959 patients with acute myocardial infarction (MI) and left ventricular ejection fraction (LVEF) ≤40%, who took either carvedilol or placebo. After an average follow-up period of 1.3 years, non-fatal MI occurrence was significantly lower in the carvedilol group (3%) than in the placebo group (6%) (hazard ratio [HR] 0.59, 95% confidence interval [CI] [0.39 – 0.90], p=0.014).5 The Carvedilol Prospective Randomized Cumulative Survival Study (COPERNICUS) recruited 2289 patients with severe heart failure and LVEF ≤25% and found similar results.4 After an average follow-up period of 10.4 months, carvedilol treatment, when compared to placebo, reduced risk of all-cause death by 35% (95% CI [19 – 48], p=0.0014).
In a large Carvedilol or Metoprolol European Trial (COMET), 3029 patients with chronic congestive heart failure were randomized to receive either carvedilol or metoprolol tartrate, a different beta blocker medication (mean follow-up duration 58 ± 6 months).6 The study found that carvedilol reduced death caused by stroke significantly more than metoprolol did (13/38, HR 0.33, 95% CI [0.18 – 0.62], p=0.0006). In addition, the carvedilol group also had a significantly lower incidence of fatal or nonfatal acute MI (HR 0.71, 95% CI [0.52 – 0.97], p=0.03).
The US Carvedilol Heart Failure Study Group conducted a double-blinded, stratified study on 1094 patients with chronic heart failure and EF ≤35%.1 Patients received digoxin, diuretics, and angiotensin converting enzyme inhibitors as background therapy, and were randomized to either the carvedilol or the placebo group. Patients were observed for the occurrence of death or hospitalization for cardiovascular reasons during the following 6 months (12 months for the group with mild heart failure). Carvedilol reduced the risk of mortality by 65% (95% CI [39% – 80%], p<0.001), finding an overall mortality rate of 3.2% and 7.8% for the carvedilol and the placebo group, respectively. The risk of hospitalization for cardiovascular causes was reduced by 27% (95% CI [3% – 45%], p=0.036) in the carvedilol group (14.1%) when compared to the placebo group (19.6%). Likewise, the carvedilol group found a 38% (95% CI [18 – 53], p<0.001) reduction in the combined risk of hospitalization or death due to cardiovascular causes compared to the placebo group. (15.8% versus 24.6%).
References
- Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334(21):1349-1355. 1996.
- Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344(22):1651-1658.
- Packer M. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation 2002; 106 (17): 2194-2199.
- Fowler MB. Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) Trial: carvedilol in severe heart failure. Am J Cardiol 2004; 93 (9, Supplement 1): 35-39.
- Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357(9266):1385-1390.
- Torp-Pedersen C, Poole-Wilson PA, Swedberg K, et al. Effects of metoprolol and carvedilol on cause-specific mortality and morbidity in patients with chronic heart failure--COMET. Am Heart J 2005; 149 (2): 370-376.