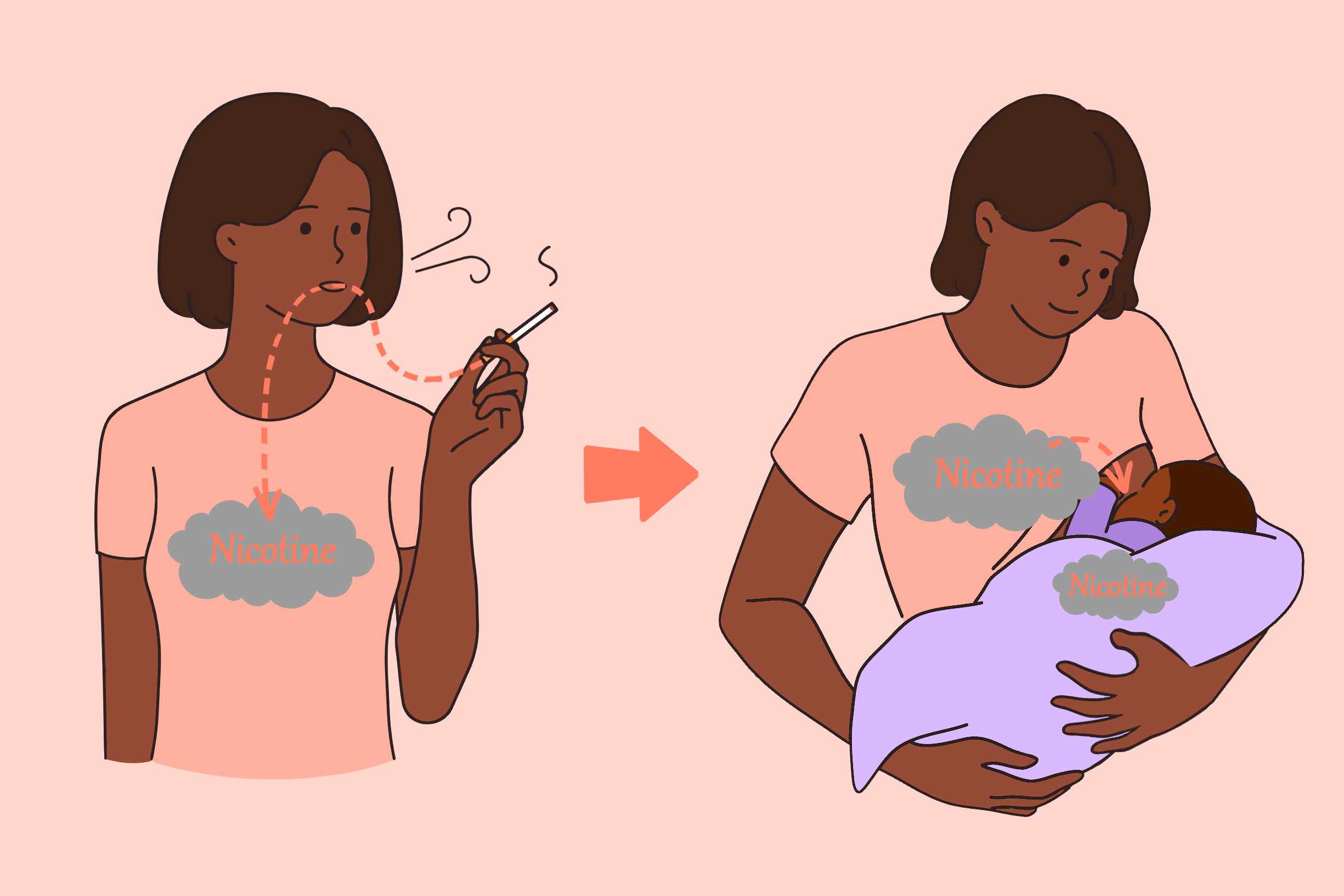
Nicotine passes into the breastmilk of individuals who use nicotine products and has a long half-life, remaining in breastmilk for upwards of 4-7 hours after use.1,2 Additionally, tobacco use during lactation can affect the nutritional content and volume of milk production. However, there are limited data evaluating the effects of nicotine use specifically as opposed to effects that may be due to smoke exposure on infants during lactation and breastfeeding. Evidence is limited, but early nicotine exposure may result in impaired sleep, reduced respiratory rate, delayed neurological development, and metabolic dysfunction.
The National Institute of Child Health and Human Development Drugs and Lactation Database (LactMed) recommends against using nicotine in any form while breastfeeding, although they cite the Academy of Breastfeeding Medicine’s (ABM) recommendation as well.3 ABM recommends that women who use nicotine products still breastfeed, with the caveat that they should be counseled to reduce or stop the use of nicotine products as much as possible while breastfeeding, especially for those who smoke or vape.4 They assert that the benefits of breastfeeding mitigate the harms of second-hand smoke and nicotine exposure. They also consider nicotine replacement products to be compatible with breastfeeding.
Similarly, the American Academy of Pediatrics does not view maternal smoking as a contraindication to breastfeeding, although individuals should be strongly encouraged to stop smoking or to minimize infant exposure.5 They consider nicotine replacement products to be compatible with breastfeeding as long as the dose is less than the number of cigarettes typically smoked. They further recommend preferential use of short-acting products such as gum or lozenges.
Nicotine in Breastmilk
A 2004 study in Stockholm, Sweden of non-smoking (n=19), smoking (n=16), and snuff-using (n=2) breastfeeding mothers examined the concentration of nicotine in their infants.2 The mean nicotine concentration in the breastmilk of smoking mothers was 44 μg/L, with concentrations at 40 minutes after smoking at 51 μg/L dropping to 21 μg/L at 7 hours. The two snuff-using mothers had higher levels of nicotine in their breastmilk at 89 and 99 μg/L within an hour of use, dropping to 47 and 57 μg/L at 7 hours. Infants of both smoking and snuff-using mothers had levels of nicotine in their urine correlated to their exposure, with a mean concentration of 0.7 μg/L (p<0.01). Two women in the nonsmoking group had detectible levels of nicotine in their breastmilk due to their exposure to secondhand smoke from their spouse’s tobacco use (mean of 28 and 13 μg/L).
A 2018 study of breastfeeding oral moist tobacco users (n=13), smokers (n=6), and nonsmokers (n=14) measured breastmilk concentrations of nicotine.1 The median concentration of nicotine in breastmilk samples collected between 5-60 minutes after tobacco use was higher for those using oral tobacco than smokers (38.7 μg/mL vs 24.0 μg/L). Nicotine could still be detected in the breastmilk of 60% of oral tobacco users 11 hours after use. Nicotine was no longer detectible in the breastmilk of smokers after four hours of use.
A 2003 study took breastmilk samples from 15 women who underwent nicotine replacement therapy, with samples collected both while they were exclusively smoking cigarettes at the beginning of the study period and later in the intervention after they had been stabilized on nicotine patches and were no longer smoking.6 Nicotine concentrations in breastmilk were not significantly different between smoking a mean of 17 cigarettes per day and the 21 mg/day patch (25.2 vs 23.0 μg/L), but concentrations decreased for the 14 mg/day and 7 mg/day patches (15.8 and 7.5 μg/L, p<0.05). Of note, all of the infants’ development was normal (assessed using the Denver Developmental Screening Test, which evaluates children’s developmental progress in personal-social, fine motor-adaptive, language, and gross motor skills).
A few studies have shown that smoking decreases the volume of milk production as well as the nutritional content of milk, although it is unclear if this is due to nicotine or other factors associated with smoking. Nutritional differences between smokers and nonsmokers include smokers having lower levels of lipids, milk fat, vitamins, and minerals and having higher levels of heavy metals.7-14
Effect on Infants
A 2007 study of 15 mother-infant pairs examined the effect of nicotine exposure on infant sleep patterns.15 Mothers smoked before breastfeeding on one test day and refrained from smoking on the other, then allowing their infants to breastfeed on demand for 3.5 hours on each test day. On test days where mothers were allowed to smoke prior to breastfeeding, women were told to smoke according to their usual habits. Thirteen women smoked one cigarette prior to breastfeeding, one smoked two cigarettes, and one smoked three. Volume of milk consumption was estimated by weighing the infants before and after feeding, and the estimated dose of nicotine delivered to the infants was calculated by multiplying the volume of milk consumption by the concentration of nicotine in the breastmilk at the start of feeding sessions. The estimated dose of nicotine delivered significantly increased from 127.1±59.8 ng/kg for the nonsmoking session to 547.9±233.0 ng/kg for the smoking session. Infants spent an average of 31.1 minutes less time sleeping during the 3.5-hour session when exposed to breastmilk after their mother smoked (84.6 vs 53.4 minutes). Additionally, the longest duration of sleep was an average of 23.2 minutes shorter (60.1 vs 36.9 minutes). There was a dose-dependent relationship between nicotine exposure and less time spent asleep.
A 1993 study of mother-infant pairs looked at respiratory markers in infants before and after breastfeeding from smoking (n=5) and nonsmoking mothers (n=5).16 Infants of smokers experienced a significant reduction in respiratory rate after feeding from 49.41 breaths per minute to 41.17 (p=0.038) while infants of nonsmokers maintained a stable respiratory rate. This change was significantly correlated with the level of nicotine in the mother’s breastmilk (p=0.004).
There is some evidence that nicotine exposure may be linked to SIDS. A 2002 case-control study (44 cases, 29 controls) found that concentrations of nicotine in the lung tissue was significantly higher among infants who had died of SIDS (19.65 ng/g vs 7.86 ng/g, p=0.0001).17 However, it is unclear if this increased risk is related to exposure to nicotine or exposure to cigarette smoke. A 1993 case-control study of 485 cases and 1,800 controls found that exposure to cigarette smoke increased the risk of SIDS.18 Among cases, 44.3% of mothers reported smoking 1-19 cigarettes in the past two weeks compared to 24.3% of controls. Similarly, 34.3% of cases had fathers who smoked 1-19 cigarettes in the past two weeks compared to 20.6% of controls. The study also examined the roll of breastfeeding, and there appeared to be either no effect or a protective influence on SIDS risk. Among smoking mothers, 23.7% of cases breastfed and 30.3% of cases didn’t breastfeed.
There are currently very few published studies examining the long-term effects of nicotine exposure on infants. There are limited data from rat models that show that early nicotine exposure may affect the endocrine system19-21 and neurological development.22-24
Nicotine Replacement Therapy
Although nicotine can be passed on to infants through breastmilk, guidelines advise that nicotine replacement therapy (NRT) is compatible with breastfeeding.4,5 The harm reduction to both the mother and infant from smoking cessation outweighs the potential risks from NRT.
References
- Nordenstam F, Lundell B, Edstedt Bonamy AK, Raaschou P, Wickström R. Snus users had high levels of nicotine, cotinine and 3-hydroxycotinine in their breastmilk, and the clearance was slower than in smoking mothers. Acta Paediatr. Jul 2019;108(7):1250-1255. doi:10.1111/apa.14602
- Dahlström A, Ebersjö C, Lundell B. Nicotine exposure in breastfed infants. Acta Paediatr. Jun 2004;93(6):810-6.
- Drugs and Lactation Database (LactMed®): Nicotine. National Institute of Child Health and Human Development. Updated 15 November 2023. Accessed 21 May, 2025. https://www.ncbi.nlm.nih.gov/books/NBK501586/
- Harris M, Schiff DM, Saia K, Muftu S, Standish KR, Wachman EM. Academy of Breastfeeding Medicine Clinical Protocol #21: Breastfeeding in the Setting of Substance Use and Substance Use Disorder (Revised 2023). Breastfeed Med. Oct 2023;18(10):715-733. doi:10.1089/bfm.2023.29256.abm
- Sachs HC. The transfer of drugs and therapeutics into human breast milk: an update on selected topics. Pediatrics. Sep 2013;132(3):e796-809. doi:10.1542/peds.2013-1985
- Ilett KF, Hale TW, Page-Sharp M, Kristensen JH, Kohan R, Hackett LP. Use of nicotine patches in breast-feeding mothers: transfer of nicotine and cotinine into human milk. Clin Pharmacol Ther. Dec 2003;74(6):516-24. doi:10.1016/j.clpt.2003.08.003
- Hopkinson JM, Schanler RJ, Fraley JK, Garza C. Milk production by mothers of premature infants: influence of cigarette smoking. Pediatrics. Dec 1992;90(6):934-8.
- Bachour P, Yafawi R, Jaber F, Choueiri E, Abdel-Razzak Z. Effects of smoking, mother's age, body mass index, and parity number on lipid, protein, and secretory immunoglobulin A concentrations of human milk. Breastfeed Med. Jun 2012;7(3):179-88. doi:10.1089/bfm.2011.0038
- Agostoni C, Marangoni F, Grandi F, et al. Earlier smoking habits are associated with higher serum lipids and lower milk fat and polyunsaturated fatty acid content in the first 6 months of lactation. Eur J Clin Nutr. Nov 2003;57(11):1466-72. doi:10.1038/sj.ejcn.1601711
- Winiarska-Mieczan A. Cadmium, lead, copper and zinc in breast milk in Poland. Biol Trace Elem Res. Jan 2014;157(1):36-44. doi:10.1007/s12011-013-9870-x
- Kwapuliński J, Wiechuła D, Fischer A. [The influence of smoking and passive smoking to occurrence of metals in breast milk]. Przegl Lek. 2004;61(10):1113-5. Wpływ palenia czynnego i biernego na zawartość metali w mleku kobiet.
- Laurberg P, Nøhr SB, Pedersen KM, Fuglsang E. Iodine nutrition in breast-fed infants is impaired by maternal smoking. J Clin Endocrinol Metab. Jan 2004;89(1):181-7. doi:10.1210/jc.2003-030829
- Ortega RM, López-Sobaler AM, Quintas ME, Martínez RM, Andrés P. The influence of smoking on vitamin C status during the third trimester of pregnancy and on vitamin C levels in maternal milk. J Am Coll Nutr. Aug 1998;17(4):379-84. doi:10.1080/07315724.1998.10718779
- Ortega RM, López-Sobaler AM, Martínez RM, Andrés P, Quintas ME. Influence of smoking on vitamin E status during the third trimester of pregnancy and on breast-milk tocopherol concentrations in Spanish women. Am J Clin Nutr. Sep 1998;68(3):662-7. doi:10.1093/ajcn/68.3.662
- Mennella JA, Yourshaw LM, Morgan LK. Breastfeeding and smoking: short-term effects on infant feeding and sleep. Pediatrics. Sep 2007;120(3):497-502. doi:10.1542/peds.2007-0488
- Stepans MB, Wilkerson N. Physiologic effects of maternal smoking on breast-feeding infants. J Am Acad Nurse Pract. May-Jun 1993;5(3):105-13. doi:10.1111/j.1745-7599.1993.tb00850.x
- McMartin KI, Platt MS, Hackman R, et al. Lung tissue concentrations of nicotine in sudden infant death syndrome (SIDS). J Pediatr. Feb 2002;140(2):205-9. doi:10.1067/mpd.2002.121937
- Mitchell EA, Ford RPK, Stewart AW, et al. Smoking and the sudden infant death syndrome. Pediatrics. 1993 1993;91(5):893-896. doi:10.1542/peds.91.5.893
- Oliveira E, Pinheiro CR, Santos-Silva AP, et al. Nicotine exposure affects mother's and pup's nutritional, biochemical, and hormonal profiles during lactation in rats. J Endocrinol. May 2010;205(2):159-70. doi:10.1677/joe-09-0430
- Bruin JE, Kellenberger LD, Gerstein HC, Morrison KM, Holloway AC. Fetal and neonatal nicotine exposure and postnatal glucose homeostasis: identifying critical windows of exposure. J Endocrinol. Jul 2007;194(1):171-8. doi:10.1677/joe-07-0050
- Santos-Silva AP, Oliveira E, Pinheiro CR, et al. Effects of tobacco smoke exposure during lactation on nutritional and hormonal profiles in mothers and offspring. J Endocrinol. Apr 2011;209(1):75-84. doi:10.1530/joe-10-0410
- Nakauchi S, Malvaez M, Su H, et al. Early postnatal nicotine exposure causes hippocampus-dependent memory impairments in adolescent mice: Association with altered nicotinic cholinergic modulation of LTP, but not impaired LTP. Neurobiol Learn Mem. Feb 2015;118:178-88. doi:10.1016/j.nlm.2014.12.007
- Eppolito AK, Bachus SE, McDonald CG, Meador-Woodruff JH, Smith RF. Late emerging effects of prenatal and early postnatal nicotine exposure on the cholinergic system and anxiety-like behavior. Neurotoxicol Teratol. May-Jun 2010;32(3):336-45. doi:10.1016/j.ntt.2009.12.009
- Son JH, Winzer-Serhan UH. Chronic neonatal nicotine exposure increases mRNA expression of neurotrophic factors in the postnatal rat hippocampus. Brain Res. Jun 30 2009;1278:1-14. doi:10.1016/j.brainres.2009.04.046